One person in my family has migraines. Below are my suggestions for the person, and the shallow literature review I did with Elicit.
My suggestions
Current medications of the person with migraines:
- Naprosyn (naproxen) for milder migraines.
- Zomig (zolmitriptan) for acute migraines.
My suggestions:
- Replace zolmitriptan with eletriptan or rizatriptan. From Fig. 3 of Xu et al. (2016), one is more likely to be pain free over 2 h using these, although they are a bit worse in terms of side effects.
- Take Coenzyme Q10. The meta-analyses of Parohan et al. (2020) and Sazali et al. (2021) present some suggestive evidence. It costs like 10 €/month (= 19.85*30/60) taking 30 capsules per month. Coenzyme Q10 may have “a few” side effects which should be monitored.
- Keep a steady intake of caffeine of less than 200 mg/d, which is up to 1 or 2 coffees per day, unless it is decaf coffee. The recommendation is based on Elicit’s summary about the effect of caffeine on migraines, although I have not looked into the evidence.
- Do not drink too much alcohol, do not stress too much, and sleep well. This is based on Elicit’s summaries about the effect of alcohol, stress and sleep on migraines. I have not looked into the evidence, but these pieces of advice intuitively make sense, and have lots of benefits anyways.
What are the best treatments for migraines?
Summary from Elicit on 6 January 2025
Recent research has explored various treatments for migraines, including traditional Chinese medicine (TCM), pharmacological interventions, and minimally invasive techniques. TCM decoctions, particularly those targeting the Shaoyang gateway, have shown promising results in clinical practice (Zhou et al., 2013). Among pharmacological options, triptans, especially eletriptan and rizatriptan, demonstrate superior pain relief compared to other NSAIDs and triptans (Xu et al., 2016). However, triptans are associated with higher odds of adverse events than non-triptans and placebo (Thorlund et al., 2017). For treatment-resistant migraines, minimally invasive techniques have been developed. Migraine surgery appears to be a cost-effective, long-term solution, significantly reducing headache frequency, severity, and duration (Chang et al., 2023). Botulinum toxin type A (BT-A) also shows efficacy in reducing headache severity and duration, although its effects are shorter-lasting compared to surgery (Chang et al., 2023). The choice of treatment should consider individual patient needs and potential side effects.
Abstracts from meta-analyses and systematic reviews from Elicit
I list the studies alphabetically. Emphasis is mine.
Acute Treatments for Episodic Migraine in Adults: A Systematic Review and Meta-analysis (Vanderpluym et al., 2021)
Importance: Migraine is common and can be associated with significant morbidity, and several treatment options exist for acute therapy.
Objective: To evaluate the benefits and harms associated with acute treatments for episodic migraine in adults [that “occur on fewer than 15 days per month”].
Data sources: Multiple databases from database inception to February 24, 2021.
Study selection: Randomized clinical trials and systematic reviews that assessed effectiveness or harms of acute therapy for migraine attacks.
Data extraction and synthesis: Independent reviewers selected studies and extracted data. Meta-analysis was performed with the DerSimonian-Laird random-effects model with Hartung-Knapp-Sidik-Jonkman variance correction or by using a fixed-effect model based on the Mantel-Haenszel method if the number of studies was small.
Main outcomes and measures: The main outcomes included pain freedom, pain relief, sustained pain freedom, sustained pain relief, and adverse events. The strength of evidence (SOE) was graded with the Agency for Healthcare Research and Quality Methods Guide for Effectiveness and Comparative Effectiveness Reviews.
Findings: Evidence on triptans and nonsteroidal anti-inflammatory drugs was summarized from 15 systematic reviews. For other interventions, 115 randomized clinical trials with 28 803 patients were included. Compared with placebo, triptans and nonsteroidal anti-inflammatory drugs used individually were significantly associated with reduced pain at 2 hours and 1 day (moderate to high SOE) and increased risk of mild and transient adverse events. Compared with placebo, calcitonin gene-related peptide receptor antagonists (low to high SOE), lasmiditan (5-HT1F receptor agonist; high SOE), dihydroergotamine (moderate to high SOE), ergotamine plus caffeine (moderate SOE), acetaminophen (moderate SOE), antiemetics (low SOE), butorphanol (low SOE), and tramadol in combination with acetaminophen (low SOE) were significantly associated with pain reduction and increase in mild adverse events. The findings for opioids were based on low or insufficient SOE. Several nonpharmacologic treatments were significantly associated with improved pain, including remote electrical neuromodulation (moderate SOE), transcranial magnetic stimulation (low SOE), external trigeminal nerve stimulation (low SOE), and noninvasive vagus nerve stimulation (moderate SOE). No significant difference in adverse events was found between nonpharmacologic treatments and sham.
Conclusions and relevance: There are several acute treatments for migraine, with varying strength of supporting evidence. Use of triptans, nonsteroidal anti-inflammatory drugs, acetaminophen, dihydroergotamine, calcitonin gene-related peptide antagonists, lasmiditan, and some nonpharmacologic treatments was associated with improved pain and function. The evidence for many other interventions, including opioids, was limited.
Canadian Headache Society systematic review and recommendations on the treatment of migraine pain in emergency settings (Orr et al., 2015)
Background
There is a considerable amount of practice variation in managing migraines in emergency settings, and evidence-based therapies are often not used first line.
Methods
A peer-reviewed search of databases (MEDLINE, Embase, CENTRAL) was carried out to identify randomized and quasi-randomized controlled trials of interventions for acute pain relief in adults presenting with migraine to emergency settings. Where possible, data were pooled into meta-analyses.
Results
Two independent reviewers screened 831 titles and abstracts for eligibility. Three independent reviewers subsequently evaluated 120 full text articles for inclusion, of which 44 were included. Individual studies were then assigned a US Preventive Services Task Force quality rating. The GRADE scheme was used to assign a level of evidence and recommendation strength for each intervention.
Interpretation
We strongly recommend the use of prochlorperazine based on a high level of evidence, lysine acetylsalicylic acid, metoclopramide and sumatriptan, based on a moderate level of evidence, and ketorolac, based on a low level of evidence. We weakly recommend the use of chlorpromazine based on a moderate level of evidence, and ergotamine, dihydroergotamine, lidocaine intranasal and meperidine, based on a low level of evidence. We found evidence to recommend strongly against the use of dexamethasone, based on a moderate level of evidence, and granisetron, haloperidol and trimethobenzamide based on a low level of evidence. Based on moderate-quality evidence, we recommend weakly against the use of acetaminophen and magnesium sulfate. Based on low-quality evidence, we recommend weakly against the use of diclofenac, droperidol, lidocaine intravenous, lysine clonixinate, morphine, propofol, sodium valproate and tramadol.
Comparative tolerability of treatments for acute migraine: A network meta-analysis (Thorlund et al., 2016)
Introduction
Migraine headache is a neurological disorder whose attacks are associated with nausea, vomiting, photophobia and phonophobia. Treatments for migraine aim to either prevent attacks before they have started or relieve attacks (abort) after onset of symptoms and range from complementary therapies to pharmacological interventions. A number of treatment-related adverse events such as somnolence, fatigue, and chest discomfort have previously been reported in association with triptans. The comparative tolerability of available agents for the abortive treatment of migraine attacks has not yet been systematically reviewed and quantified.
Methods
We performed a systematic literature review and Bayesian network meta-analysis for comparative tolerability of treatments for migraine. The literature search targeted all randomized controlled trials evaluating oral abortive treatments for acute migraine over a range of available doses in adults. The primary outcomes of interest were any adverse event, treatment-related adverse events, and serious adverse events. Secondary outcomes were fatigue, dizziness, chest discomfort, somnolence, nausea, and vomiting.
Results
Our search yielded 141 trials covering 15 distinct treatments. Of the triptans, sumatriptan, eletriptan, rizatriptan, zolmitriptan, and the combination treatment of sumatriptan and naproxen were associated with a statistically significant increase in odds of any adverse event or a treatment-related adverse event occurring compared with placebo. Of the non-triptans, only acetaminophen was associated with a statistically significant increase in odds of an adverse event occurring when compared with placebo. Overall, triptans were not associated with increased odds of serious adverse events occurring and the same was the case for non-triptans. For the secondary outcomes, with the exception of vomiting, all triptans except for almotriptan and frovatriptan were significantly associated with increased risk for all outcomes. Almotriptan was significantly associated with an increased risk of vomiting, whereas all other triptans yielded non-significant lower odds compared with placebo. Generally, the non-triptans were not associated with decreased tolerability for the secondary outcomes.
Discussion
In summary, triptans were associated with higher odds of any adverse event or a treatment-related adverse event occurring when compared to placebo and non-triptans. Non-significant results for non-triptans indicate that these treatments are comparable with one another and placebo regarding tolerability outcomes.
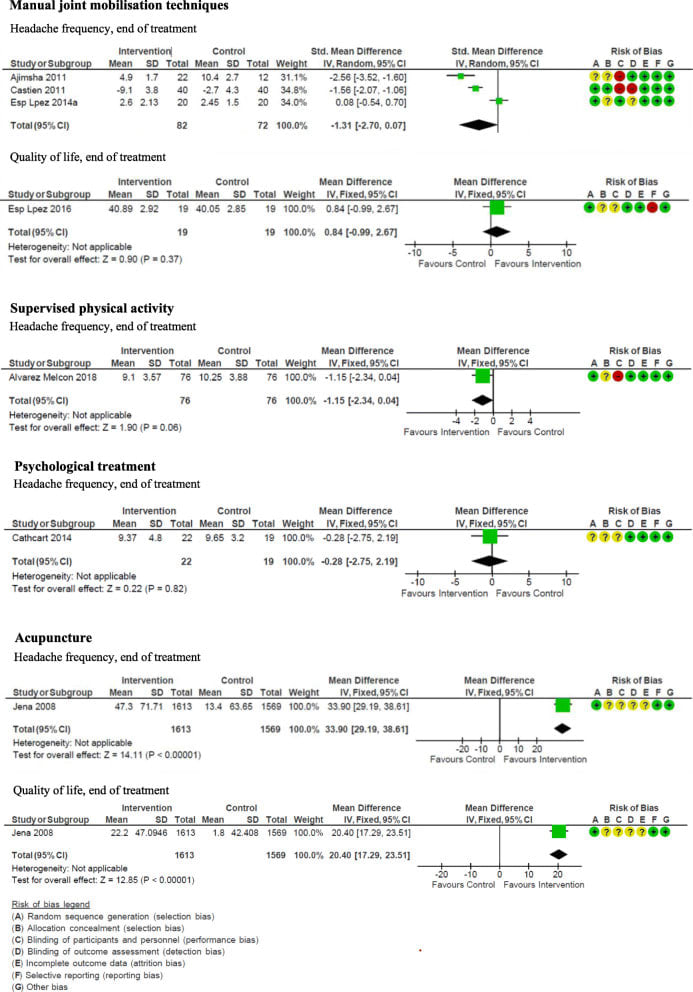
Manual joint mobilisation techniques, supervised physical activity, psychological treatment, acupuncture and patient education in migraine treatment. A systematic review and meta-analysis (Beier et al., 2021)
Background: Many people suffering from migraine combine pharmacological and non-pharmacological treatments. The purpose of this systematic review is to provide an updated guideline for some widely used non-pharmacological treatment options for migraine.
Methods: We conducted a systematic literature review of randomized studies of adults with migraine treated with manual joint mobilisation techniques [“all manual techniques, mobilisation or manipulation within the normal range of motion of the joint, aimed at affecting the joints, muscles and connective tissues of the neck, chest and lower back”], supervised physical activity [“planned, repeated and structured physical activity”], psychological treatment [“approaches that address self-efficacy to decrease negative effect of reduced functioning and improve quality of life despite headache pain and headache related disability”], acupuncture [“treatment where thin needles are inserted into the body including dry-needling and trigger point acupuncture excluding electroacupuncture”] and patient education [“improving the understanding of the disorder and treatment options”]. The main outcomes measured were days with headache and quality of life. Recommendations were formulated based on the Grade of Recommendation, Assessment, Development and Evaluation (GRADE) approach including patient preferences based on expert opinion and questionnaire data.
Results: The overall level of certainty of the evidence was low to very low. Manual therapy techniques and psychological treatment did not change the studied outcomes. Supervised physical activity might have a positive impact on quality of life, acupuncture on headache frequency, intensity, quality of life and the use of attack-medicine. Patient education might improve self-rated health and quality of life and increase the number of well-informed patients.
Conclusion: Based on observed effects, the lack of serious adverse events, and patients' preferences, we make weak recommendations for considering the investigated interventions as a supplement to standard treatment.
Vasco. 5 of the 6 meta-analyses only cover one estimate! Lol.
Network meta-analysis of migraine disorder treatment by NSAIDs and triptans (Xu et al., 2016)
Migraine is a neurological disorder resulting in large socioeconomic burden. This network meta-analysis (NMA) is designed to compare the relative efficacy and tolerability of non-steroidal anti-inflammatory agents (NSAIDs) and triptans.
We conducted systematic searches in database PubMed and Embase. Treatment effectiveness was compared by synthesizing direct and indirect evidences using NMA. The surface under curve ranking area (SUCRA) was created to rank those interventions.
Eletriptan and rizatriptan are superior to sumatriptan, zolmitriptan, almotriptan, ibuprofen and aspirin with respect to pain-relief. When analyzing 2 h-nausea-absence, rizatriptan has a better efficacy than sumatriptan, while other treatments indicate no distinctive difference compared with placebo. Furthermore, sumatriptan demonstrates a higher incidence of all-adverse-event compared with diclofenac-potassium, ibuprofen and almotriptan.
This study suggests that eletriptan may be the most suitable therapy for migraine from a comprehensive point of view. In the meantime ibuprofen may also be a good choice for its excellent tolerability. Multi-component medication also attracts attention and may be a promising avenue for the next generation of migraine treatment.
Nonpharmacologic Treatments for Chronic and Episodic Migraine: A Systematic Review and Meta-Analysis (Chang et al., 2023)
Background: Minimally invasive techniques for treatment-resistant migraine have been developed on recent insights into the peripheral pathogenesis of migraines. Although there is a growing body of evidence supporting these techniques, no study has yet compared the effects of these treatments on headache frequency, severity, duration, and cost.
Methods: PubMed, Embase, and Cochrane Library databases were searched to identify randomized placebo-controlled trials that compared radiofrequency ablation, botulinum toxin type A (BT-A), nerve block, neurostimulation, or migraine surgery to placebo for preventive treatment. Data on changes from baseline to follow-up in headache frequency, severity, duration, and quality of life were analyzed.
Results: A total of 30 randomized controlled trials and 2680 patients were included. Compared with placebo, there was a significant decrease in headache frequency in patients with nerve block ( P = 0.04) and surgery ( P < 0.001). Headache severity decreased in all treatments. Duration of headaches was significantly reduced in the BT-A ( P < 0.001) and surgery cohorts ( P = 0.01). Quality of life improved significantly in patients with BT-A, nerve stimulator, and migraine surgery. Migraine surgery had the longest lasting effects (11.5 months) compared with nerve ablation (6 months), BT-A (3.2 months), and nerve block (11.9 days).
Conclusions: Migraine surgery is a cost-effective, long-term treatment to reduce headache frequency, severity, and duration without significant risk of complication. BT-A reduces headache severity and duration, but it is short-lasting and associated with greater adverse events and lifetime cost. Although efficacious, radiofrequency ablation and implanted nerve stimulators have high risks of adverse events and explantation, whereas benefits of nerve blocks are short in duration.
Patient Related Outcome Measures Dovepress Patient Outcome in Migraine Prophylaxis: the Role of Psychopharmacological Agents (Pompili et al., 2010)
Introduction: Migraine is a serious illness that needs correct treatment for acute attacks and, in addition, a treatment prophylaxis [to prevent disease], since patients with migraine suffer during acute attacks and also between attacks.
Methods: A systematic review of the most relevant clinical trials of migraine headache and its epidemiology, pathophysiology, comorbidity, and prophylactic treatment (medical and nonmedical) was carried out using “Medline” and “PsychINFO” from 1973 to 2009. Approximately 110 trials met our inclusion criteria and were included in the current review.
Results: The most effective pharmacological treatment for migraine prophylaxis is propranolol and anticonvulsants such as topiramate, valproic acid, and amitriptyline. Nonmedical treatments such as acupuncture, biofeedback, and melatonin have also been proposed. Peripheral neurostimulation has been suggested for the treatment of chronic daily headache that does not respond to prophylaxis and for the treatment of drug-resistant primary headache. The majority of the pharmacological agents available today have limited efficacy and may cause adverse effects incompatible with long-term use.
Limitations: The review was limited by the highly variable and often insufficient reporting of the complex outcome data and by the fact that migraine prophylaxis trials typically use headache diaries to monitor the course of the disease. The results of the different studies were also presented in different ways, making comparison of the results difficult.
Discussion: An adequate prophylaxis is crucial in reducing disability and preventing the evolution of the problem into a chronic progressive illness. The implications of the present findings were discussed.
What is the best diet for migraines?
Summary from Elicit on 6 January 2025
Recent research suggests that dietary interventions may be effective in managing migraines. The ketogenic diet (KD) has shown promise in reducing the frequency, duration, and severity of migraine headaches in adults (Gazerani, 2023; Caminha et al., 2021). A systematic review found that most studies reported KD reduced migraine attacks with few adverse effects, although the evidence quality was low (Caminha et al., 2021). Another review indicated that all forms of ketogenic therapy, including very low-calorie ketogenic diet, modified Atkins diet [a low carb diet], and exogenous beta-hydroxybutyrate administration, had significant effects on migraine management (Neri et al., 2023). Additionally, following an anti-inflammatory diet was associated with lower frequency and severity of migraine headaches (Alqahtani et al., 2024). However, more well-designed studies are needed to establish causality and understand underlying mechanisms. Personalized dietary plans, considering individual triggers and lifestyle factors, are recommended for optimal migraine management (Gazerani, 2023).
Abstracts from meta-analyses and systematic reviews from Elicit
I list the studies alphabetically. Emphasis is mine.
Efficacy and tolerability of the ketogenic diet and its variations for preventing migraine in adolescents and adults: a systematic review (Caminha et al., 2022)
Context: Migraine is a headache of variable intensity that is associated with focal and systemic symptoms. A ketogenic diet (KD), a very-low-carbohydrate diet with a proportional increase in fat, causes brain metabolic alterations, which could be beneficial for some neurologic conditions.
Objective: A systematic review was conducted to assess the efficacy and tolerability of KD in preventing migraine in adolescents and adults.
Data sources: The Preferred Reporting Items for Systematic Reviews and Meta-Analyses standard was used to review articles found in the PubMed, EMBASE, Scopus, Web of Science, LILACS, LIVIVO, Science Direct, and Cochrane Central Register of Controlled Trials databases. The Google Scholar, DOAJ, ProQuest, and OpenGrey databases were included.
Data extraction: The population, intervention, comparison, outcome, and study design strategy included assessing the quality of the evidence using Grading of Recommendations Assessment Development and Evaluation and the risk of bias after applying the JBI critical appraisal tools.
Data analysis: Most of the 10 selected studies reported that KD reduced the number and severity of migraine attacks in patients, with few reported adverse effects. The evidence on the effectiveness of the KD is low, so whether the final effect is due to the treatment remains inconclusive.
Conclusions: This study represents an initial effort to systematize information on the efficacy and tolerability of KD and its variations in the prevention of migraine.
Dietary inflammatory potential and severe headache or migraine: a systematic review of observational studies (Alqahtani et al., 2024)
Objectives: We conducted the current systematic review to investigate the association between dietary inflammatory index (DII) and severe headaches or migraine among adults via synthesizing observational evidence.
Method: We conducted a systematic literature search of observational studies through PubMed, Scopus, and Web of Science databases from inception until July 2024. The PECO framework was implemented to select eligible studies as follows: Population (adults with severe headache or migraine), Exposure (individuals with the highest adherence to a pro-inflammatory diet), Comparison (individuals with the lowest adherence to a pro-inflammatory diet), Outcome (risk of developing severe headache or migraine, headaches frequency, duration, severity, and migraine-related disability).
Results: After reviewing six studies involving 31,958 individuals, we found that following an anti-inflammatory diet is associated with a lower frequency and severity of migraine headaches. Additionally, our research revealed that individuals with migraines tend to have lower adherence to an anti-inflammatory diet when compared to people without migraines. Surprisingly, adherence to a pro-inflammatory diet was linked to a reduced risk of chronic daily headaches.
Conclusion: Present findings imply a negative link between an inflammatory diet and severe headaches or migraine. However, further well-designed longitudinal studies are needed to interpret the causality and shed light on the underlying mechanisms.
Effects of dietary supplementations and herbs on migraine - a systematic review (Rehman et al., 2019)
Background
Migraine is a disabling disease and conventional treatment has many side effects. Dietary supplements and various herbs have reported valuable effects on migraine.
Aim
The present study systematically review the effects of these dietary supplements and herbs on migraine.
Methods
The literature search was done on electronic databases PubMed, Google Scholar and Science direct (2005–2015). The quality of articles was assessed through a criteria list of methodological quality assessment of randomized controlled trials (RCTs). The papers got C50 points considered to be of good quality methodology. The maximum score was 100.
Results
Fourteen RCTs on migraine were included in this review. The range of quality score varied from 37 to 65 points.
Conclusion
Various RCTs suggested that dietary and vitamin supplementation and different herbs might be effective in treatment of migraine. Evaluated RCTs have various methodological shortcomings. So, a firm conclusion can’t be made for the efficacy of dietary supplementation and herbs in the treatment of migraine.
Vasco. I could not easily find the full text.
Ketosis and migraine: a systematic review of the literature and meta-analysis (Neri et al., 2023)
Introduction: Headaches are a prevalent disorder worldwide, and there is compelling evidence that certain dietary interventions could provide relief from attacks. One promising approach is ketogenic therapy, which replaces the brain's glucose fuel source with ketone bodies, potentially reducing the frequency or severity of headaches.
Aim: This study aims to conduct a systematic review of the scientific literature on the impact of ketosis on migraine, using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) method.
Results: After a careful selection process and bias evaluation, 10 articles were included in the review, primarily from Italy. The bias assessment indicated that 50% of the selected articles had a low risk of bias in all domains, with the randomization process being the most problematic domain. Unfortunately, the evaluation of ketosis was inconsistent between articles, with some assessing ketonuria, some assessing ketonemia, and some not assessing ketosis levels at all. Therefore, no association could be made between the level of ketosis and the prevention or reduction of migraine attacks. The ketogenic therapies tested in migraine treatments included the very low-calorie ketogenic diet (VLCKD, n = 4), modified Atkins diet (MAD, n = 3), classic ketogenic diet (cKDT, n = 2), and the administration of an exogenous source of beta-hydroxybutyrate (BHB). The meta-analysis, despite reporting high heterogeneity, found that all interventions had an overall significant effect (Z = 9.07, p < 0.00001; subgroup differences, Chi2 = 9.19, dif = 3, p = 0.03; I2, 67.4%), regardless of the type of endogenous or exogenous induction of ketosis.
Conclusion: The initial findings of this study suggest that metabolic ketogenic therapy may provide some benefit in treating migraines and encourage further studies, especially randomized clinical trials with appropriate and standardized methodologies. The review strongly recommends the use of the adequate measurement of ketone levels during ketogenic therapy to monitor adherence to the treatment and improve knowledge of the relationship between ketone bodies and efficacy.
Vasco. I think the evidence for benefits is very weak. The sample size of the estimates included in the meta-analyses ranges from 18 to 45 (see Figure 2), only one of the meta-analysed studies was a randomised controlled trial, and publication bias was not assessed.
Other abstracts
I list the studies alphabetically. Emphasis is mine.
Coenzyme Q10 supplementation for prophylaxis in adult patients with migraine-a meta-analysis (Sazali et al., 2021)
Objective: To determine the effects of coenzyme Q10 (CoQ10) for reduction in the severity, frequency of migraine attacks and duration of headache in adult patients with migraine.
Design: Systematic review and meta-analysis.
Data sources: Cochrane Central Register of Controlled Trials, CENTRAL, MEDLINE, EMBASE, Cumulative Index to Nursing and Allied Health Literature (CINAHL) and Psychological Information Database (PsycINFO) from inception till December 2019.
Study selection: All randomised control trials comparing CoQ10 with placebo or used as an adjunct treatment included in this meta-analysis. Cross-over designs and controlled clinical trials were excluded.
Data synthesis: Heterogeneity at face value by comparing populations, settings, interventions and outcomes were measured and statistical heterogeneity was assessed by means of the I2 statistic. The treatment effect for dichotomous outcomes were using risk ratios and risk difference, and for continuous outcomes, mean differences (MDs) or standardised mean difference; both with 95% CIs were used. Subgroup analyses were carried out for dosage of CoQ10 and if CoQ10 combined with another supplementation. Sensitivity analysis was used to investigate the impact risk of bias for sequence generation and allocation concealment of included studies.
Results: Six studies with a total of 371 participants were included in the meta-analysis. There is no statistically significant reduction in severity of migraine headache with CoQ10 supplementation. CoQ10 supplementation reduced the duration of headache attacks compared with the control group (MD: -0.19; 95% CI: -0.27 to -0.11; random effects; I2 statistic=0%; p<0.00001). CoQ10 usage reduced the frequency of migraine headache compared with the control group (MD: -1.52; 95% CI: -2.40 to -0.65; random effects; I2 statistic=0%; p<0.001).
Conclusion: CoQ10 appears to have beneficial effects in reducing duration and frequency of migraine attack.
The Efficacy of Herbal Supplements and Nutraceuticals for Prevention of Migraine: Can They Help? (Kaur et al., 2021)
Migraine is a common neurological disorder associated with or without aura. Although the pathophysiology of migraine is not very well understood, pro-inflammatory cytokines and oxidative stress biomarkers are found to be increased in migraine. Multiple studies have been done to see if alternative medicine such as herbal supplements and nutraceuticals are effective in the prevention and treatment of migraine headaches. This review aimed to evaluate the effect of supplements like coenzyme Q10, riboflavin (vitamin B2), feverfew, and magnesium on the frequency, severity, and duration of migraine attacks.
We performed a thorough literature search using mainly PubMed. We included studies published in the last 10 years, those conducted among adult human participants 18-65 years of age, and those published in the English language. Based on the articles selected for the final review, we concluded that herbal supplements and nutraceuticals help reduce the frequency of migraine headaches; however, mixed results were seen regarding the severity and duration of headaches. Moreover, there were no concerning side effects with these supplements. Therefore, physicians can suggest herbal supplements to patients who experience adverse effects from pharmaceutical drugs and desire a more natural treatment.
Vasco. It looks like coenzyme Q10 is the most promising supplement. It is supported by the meta-analyses of Parohan et al. (2020) and Sazali et al. (2021), which are the only 2 mentioned in the study. Their abstracts are in this section.
Effect of coenzyme Q10 supplementation on clinical features of migraine: a systematic review and dose-response meta-analysis of randomized controlled trials (Parohan et al., 2020)
Objective: Coenzyme Q10 is an antioxidant and an essential mitochondrial cofactor which has been suggested to improve the clinical features of migraine. Several randomized clinical trials have examined the effects of Coenzyme Q10 on migraine with inconclusive results. The aim of this systematic review and meta-analysis was to evaluate the impact of Coenzyme Q10 supplementation on the frequency, severity, and duration of migraine attacks.
Methods: A systematic review of the literature was conducted using ISI Web of Science, PubMed, Cochrane library and Scopus to identify eligible studies up to April 2018. Studies included were randomized clinical trials of Coenzyme Q10 supplementation that reported the frequency, severity, or duration of migraine attacks as a primary outcome. A meta-analysis of eligible studies was performed using the fixed effects model or the random effects model to estimate pooled effect size.
Results: Four randomized clinical trials with 221 participants were included. Coenzyme Q10 supplementation significantly reduced the frequency of migraine attacks (weighted mean difference: -1.87 attacks/month, 95% CI: -2.69 to -1.05, p < 0.001) without significant heterogeneity among the studies (I 2 = 36.6%, p = 0.192). Coenzyme Q10 supplementation had no significant effect on severity (weighted mean difference: -2.35 visual analog scale score, 95% CI: -5.19 to 0.49, p = 0.105) and duration of migraine attacks (weighted mean difference: -6.14 h, 95% CI: -13.14 to 0.87, p = 0.086) with high heterogeneity.
Conclusion: Pooled analyses of available randomized clinical trials suggest that Coenzyme Q10 supplementation may reduce the frequency of migraine attacks per month without affecting the severity or duration of migraine attacks.
What is the effect of caffeine on migraines?
Summary from Elicit on 11 January 2025
Caffeine's role in migraines is complex, acting as both a potential trigger and a treatment. While some studies report caffeine as a migraine trigger in 2-30% of participants (Nowaczewska et al., 2020), others suggest that pre-migraine symptoms may lead to caffeine consumption rather than caffeine directly triggering migraines (Alstadhaug & Andreou, 2019). Caffeine's therapeutic effects in migraine treatment include vascular modulation, adenosine antagonism, and inhibition of certain inflammatory mediators (Ciuba et al., 2024). However, chronic caffeine consumption may increase migraine burden, while withdrawal can trigger migraine-like headaches (Alstadhaug & Andreou, 2019). Interestingly, one study found that caffeine abstinence improved acute migraine treatment efficacy (Lee et al., 2016). Current evidence does not support recommending universal caffeine cessation for migraine patients, but limiting intake to 200 mg daily and maintaining consistent consumption is advised to avoid withdrawal-induced attacks (Nowaczewska et al., 2020).
What is the effect of alcohol on migraines?
Summary from Elicit on 11 January 2025
Alcohol is commonly reported as a migraine trigger, with about one-third of patients identifying it as an occasional trigger (Panconesi, 2008). However, prospective studies suggest its importance as a trigger may be overestimated (Panconesi, 2008). Red wine is often cited as the primary culprit, though other alcoholic beverages can also provoke attacks (Panconesi, 2008; Nicolodi & Sicuteri, 1999). The mechanism behind alcohol-induced migraines is complex, potentially involving vasodilation, dehydration, and stimulation of meningeal nociceptors (García-Azorín, 2022). Interestingly, recent research indicates that moderate alcohol consumption may not significantly increase migraine risk, with no elevated probability of an attack the day after drinking (García-Azorín, 2022). Stress appears to play a more significant role in triggering migraines, particularly when combined with alcohol consumption (Nicolodi & Sicuteri, 1999). These findings suggest that the relationship between alcohol and migraines is more nuanced than previously thought, and moderate consumption may be tolerable for some patients.
What is the effect of stress on migraines?
Summary from Elicit on 11 January 2025
Research consistently shows that stress plays a significant role in migraine, with 50-80% of patients reporting it as a trigger for their attacks (Radat, 2013; Sauro & Becker, 2009). Stress can initiate migraines in predisposed individuals, contribute to migraine chronification, and create a vicious cycle where migraine attacks themselves act as stressors (Kajal et al., 2017; Sauro & Becker, 2009). Studies have found that migraineurs experience higher levels of stress and anxiety compared to non-migraineurs, often above clinical thresholds (Wacogne et al., 2003). The stress-migraine interaction may result from biochemical changes related to the physiological stress response or psychological responses to stressors (Sauro & Becker, 2009). Stress management therapies, such as relaxation techniques, biofeedback, and cognitive-behavioral therapies, have shown effectiveness in migraine prophylaxis, particularly when combined with pharmacological treatments (Radat, 2013). Understanding and managing the stress-migraine relationship is crucial for improving the quality of life for migraine sufferers.
What is the effect of sleep on migraines?
Summary from Elicit on 11 January 2025
Sleep and migraine have a complex, bidirectional relationship. Sleep disturbances can both trigger and relieve migraine attacks (Inamorato et al., 1993). Chronic migraine patients often experience poor sleep quality, which can lead to migraine chronification and reduced quality of life (Saçmacı et al., 2022). Insufficient sleep may alter cortical excitability, particularly in the periods before and after migraine attacks, potentially causing dysfunction in GABAergic inhibition (Mykland et al., 2023). The connection between sleep and migraine may involve common underlying mechanisms, including shared brainstem-cortical networks, signaling molecules like serotonin and dopamine, and the glymphatic system (Vgontzas & Pavlović, 2018). Various sleep disorders, such as insomnia, obstructive sleep apnea, and parasomnias, have been associated with migraine. The hypothalamus has been identified as a key mediator in both sleep physiology and migraine pathophysiology, further supporting the intricate relationship between these two phenomena (Vgontzas & Pavlović, 2018).