Vida Plena (meaning ‘a flourishing life’ in Spanish) is a new nonprofit organization based in Quito, Ecuador. Our mission is to build strong mental health in low-income and refugee communities, who otherwise would have no access to care. We provide evidence-based depression treatment which is highly cost-effective and scalable.
In this post, we:
- Share how we got started
- Make the case for why you should care about mental health
- Demonstrate the evidence base for the solution we are using
- Hope to make you really excited about Vida Plena’s goals and upcoming plans
We are proud to highlight that Vida Plena completed the 2022 Charity Entrepreneurship (CE) Incubator program, making it the first CE-incubated organization to operate in Latin America. We (myself, Joy Bittner and my co-founder, Anita Kaslin) are exceptionally grateful for their on-going support and for the network of seed funders who are making this work possible.
We are also excited to contribute to the EA community locally, as Vida Plena is one of the very first EA-aligned organizations implementing within Latin America.
For the very effective altruist, a TLDR summary:
The problem: The World Health Organization (WHO) estimates that 5% of people in Latin America have depression, however, a lack of prioritization means that more than 3 out of 4 people in Latin America go untreated. Ecuador, in particular, has some of the highest rates of depression in the region: causing 8.3% of the total years lived with disability (YLD).
The solution: Vida Plena’s intervention is based on an evidence-based therapy which is recommended by the WHO as a first-line treatment for depression in low-income settings (WHO, 2020). This program is highly cost-effective as it is delivered by non-specialist community members, which a systematic review of 27 studies found that non-specialists can effectively administer therapy.
How you can know this will be impactful: We are replicating a proven program model. This intervention has been implemented in places such as in Uganda, Tanzania, and Lebonon, were studies have show that 80% of people see significant reductions in their depression. This success has led to Founders Pledge (Halstead, 2019) and the Happier Lives Institute (HLI, 2022) to recommend organizations using this therapy model for funders looking for places to provide high-impact donation. Despite an extensive body of evidence demonstrating the effectiveness and impact, Vida Plena is the first to introduce this model to Latin America.
Current status: we have certified 10 local community facilitators and are currently running a pilot program with 10 support groups. We’re looking forward to sharing the results of the pilot early 2023, but we predict that when operating at scale, it will cost $17 to improve a recipient’s wellbeing by one wellbeing-adjusted life year (WELLBY). For a comparison, this is 8 times more cost-effective than GiveDirectly (see our full predictive CEA here).
How you can help:
- Stay in touch and spread the word: generous introductions and people sharing time-sensitive information have made all this possible. sign-up to stay in touch here so we can send you news about what's happening and ways you can help
- Support us financially: we plan to treat almost 3,000 people in 2023, but have yet to secure the full funding to do so. We would be so grateful if you decide to donate or email us at joy@vidaplena.global
Section 1: How Vida Plena got started
True story - I started Vida Plena because I saw a Facebook post. Specifically, I saw a post about a new type of mental health program being run by local ‘grandmas’ in Africa. And the more I read through the multiple published studies demonstrating the evidence of its effectiveness, the more I was convinced that I need to create something similar in Ecuador, my adopted home where I have been living for the past decade.
Ecuador, as a middle-income country, is frequently overlooked by big-money development institutions. However its middle-income status masks a huge section of the population which is living on the edge of financial ruin - meaning spending money on mental health care would mean having to cut back on food or other basic needs. The result is people with depression just struggle on, somehow getting by, but not thriving. This is something I have personally watched happen time and time again as I describe in my post on the EA for Christians forum.
It was these experiences, plus 15 years working with traditional development programs across Latin America and seeing their lack of rigorous commitment to impact and evidence, that convinced me of the need to attempt to replicate the impact-driven successes I had been reading about. I began laying the groundwork for Vida Plena in early 2022, and a few months later, Anita Kaslin, an Ecuadorian psychologist with 10 years of experience, joined me as co-founder. Together, we were accepted to the Charity Entrepreneurship Incubator as part of this summer’s 2022 cohort.

Image: Gabi Pozo (our first team member), Anita, and myself
To date, Vida Plena has accomplished the following:
- Signed formal partnership with the Columbia University Global Mental Health Lab in NYC to provide initial training and on-going supervision
- Received official nonprofit status in the US
- Developed a research partnership with a top Ecuadorian university to conduct an impact evaluation in 2023
- Launched of our pilot program, starting in fall 2022

Image: Day 2 of group facilitator trainings
Currently, as part of the pilot, we:
- Have formed a team of 12 committed community members who have completed 100+ hours of training to become certified interpersonal therapy group facilitators
- Are running 10 depression support groups (8 session per cycle) in neighborhood locations across Quito
- Have demonstrated local community support through the signing of collaboration agreements with implementation partners
- Are gathering baseline and endline data as part of a feasibility study in collaboration with Columbia University
Based on the results of StrongMinds, we expect that at least 85% of people who complete treatment will see a significant reduction in their depression. We look forward to sharing the results of the pilot in early 2023.

Image: our incredible (goofy) team of group facilitators in Quito
Section 2: Mental health problems are quality of life problems
The term ‘mental health’ has recently become a bit of a buzz-word, and overused to the point that I occasionally find myself vaguely nauseated by the trite repetition of the platitudes used. While numbers and statistics can be a useful short-handway of trying to describe a situation, if you have ever personally lived through a time of terrible distress, or watched by as a close friend or family member went through one, you already know why this matters. In short, poor mental health means that everything else in life you hope to do becomes exceptionally hard, sometimes impossible. Worse is the terror that it may never improve.
Mental health illness is one of the most neglected health problems in the world (Walker et al., 2021; WHO 2020) and depression is the most common problem people face. Even before the major stressors of the pandemic, depressive disorders accounted for the largest proportion of global mental disorder DALYs (37·3% [32·3–43·0]) (Lancet, 2019).
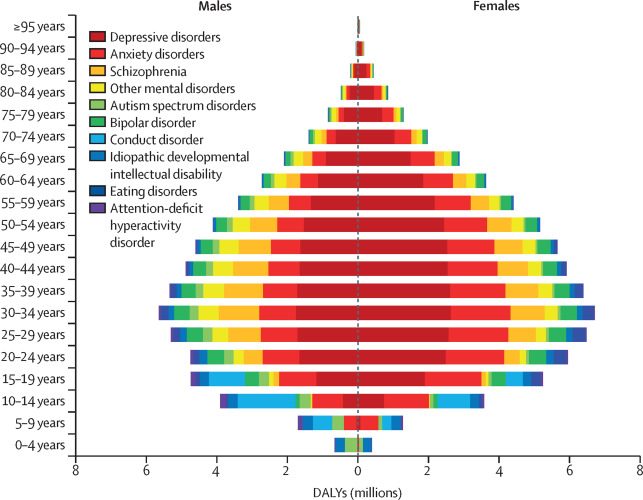
(Image source: The Lancet, 2019)
However, in most low and middle income countries (LMICs) investment in mental health has often been ignored, being considered something of a ‘luxury’ in comparison to other more high profile diseases (Freeman, 2022). This is a short-sighted budgeting strategy, as for every $1 invested in scaling up treatment for depression leads to a return of $4 in better health and ability to work.
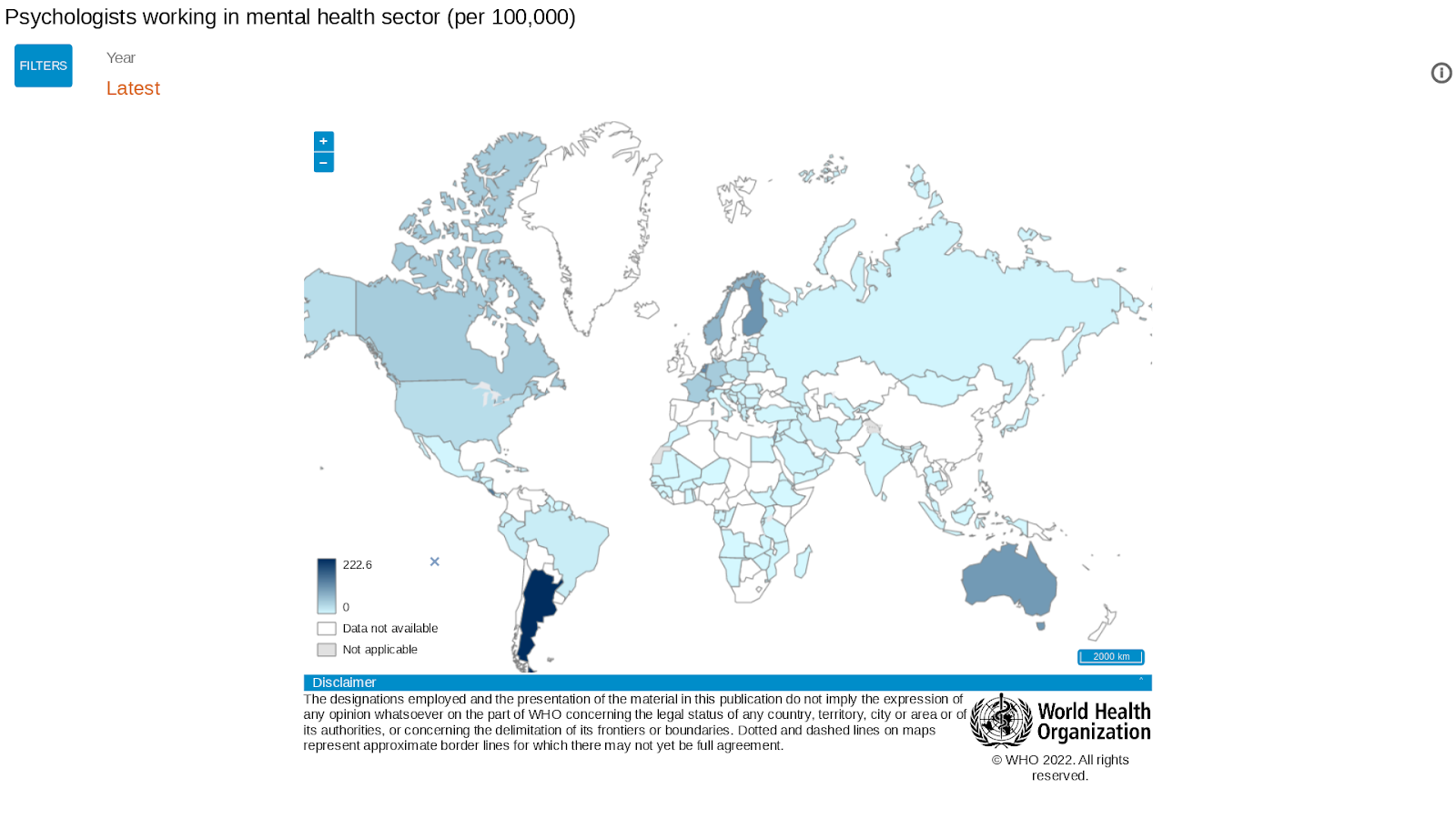
(image source: WHO, 2022)
The negative impact of poor mental health is far-reaching
Marked by intense feelings of hopelessness and an inability to enjoy normal life, depression affects almost every aspect of daily life, including:
- More relationship conflicts and higher rates of divorce
- Poor physical health outcomes, including higher probability of developing a physical disability
- 20x greater risk for suicide than the general population
One of the underappreciated effects of depression is the negative impact on people’s ability to navigate daily economic and life choices. Depression impairs attention, memory, information processing and decision-making. It also lowers cognitive flexibility (the ability to adapt strategies to changing situations) and executive functioning (the ability to complete the steps to get something done) (Hammer, 2009).
Beyond the affected individual, the broader effects of poor mental health on society at large are numerous. Globally, it is estimated that:
- 12 billion productive days are lost each year due to depression causing absenteeism for both patients and their caregivers
- $2.5 trillion is the estimated annual cost of mental health illness due to the loss of economic productivity and the direct costs of treatment,
- This cost is estimated to grow to $6.0 trillion per year by 2030
What’s the mental health situation like in Latin America?
First off, to dispel any notions that depression is simply caused by poverty or the modern-day lifestyle of developed countries, pre-pandemic estimates of the 12-month prevalence of a major depressive disorder are almost identical between high-income countries (5.5%) and LMICs (5.9%) (Lancet, 2018). Depression is found around the globe, in rich and poor places.
While it’s difficult to find updated rates of depression in Latin America (Errazuriz, 2021), pre-pandemic estimates found that, depressive disorders are the largest cause of disability alone, and combined with mortality, account for 3.4% of total DALYs and 7.8% of total YLDs (PAHO, 2019). Furthermore, the latest available estimates suggest that 15% of children and adolescents aged 10-19 in Latin America – around 16 million people – live with a diagnosed mental disorder. Every day, more than 10 adolescents lose their lives to suicide in the region (UNICEF, 2021).
Anecdotally, since the pandemic, even the fruit vendors in the market talk to me about their stress and depression being much worse. These personal experiences are backed up by a Lacet study which found that in Latin America, rates of depression increased by 35% post-pandemic (as compared to 27% in high-income countries).
Section 3: Evidence-based treatment that scales
Vida Plena has partnered with the Columbia University Global Mental Health Lab to implement their community-based model of group interpersonal therapy (g-IPT). This model is recommended by the WHO as the first line of treatment for depression in low-income settings. The basic structure of the program consists of groups of 6-8 people who meet weekly for a total of 8 sessions. The meetings happen in people’s local neighborhoods at community centers, churches, and the offices of partner organizations.
Interpersonal therapy is considered by mental health experts to be a highly effective therapy for depression (see the meta-analysis by Cuijpers et al., 2011). It is based on helping people better understand the interplay between their depression symptoms and the events in their lives, and then learning skills to better manage their depression - all while building stronger support networks.
A second key aspect of Vida Plena’s model is based on training local community members, who are non-specialists, how to provide effective depression treatment (the official jargon for this strategy is called ‘task-shifting’). This means our intervention is affordable and can be highly scalable (WHO, 2008). In one of the earliest examples of community-based group interpersonal therapy in Uganda, Bolton et al. (2003; Bass et al., 2006) found that it significantly reduced depression compared to a control group, with an absolute reduction of depression symptoms in 75% of participants even six months following the end of treatment.
More recently, the nonprofit StrongMinds, which works in Uganda and Zambia has continued to demonstrate the huge impacts that can be achieved through task-shifted g-IPT. In just over ten years, they have successfully reduced depression symptoms in more than 150,000 women. Because of this impressive track record, StrongMinds is the Happier Lives Institute’s top charity recommendation for 2022 and HLI estimates them to be ~10x more cost-effective than GiveDirectly.
Section 4: Plans for growth and scaling - because all people deserve to have a flourishing life
Despite an extensive body of evidence demonstrating the effectiveness and impact of this intervention model, it has not been implemented in Latin America. As such, the goal of Vida Plena is to replicate successes of previous task-shifted g-IPT interventions, such as StrongMinds, in Latin America.
We are confident that we will be able to achieve this goal as Vida Plena has been trained and certified in g-IPT by the very same team of mental health experts from the Global Mental Health Lab at Columbia University, who also originally trained StrongMinds when they first began. The Columbia University team has also committed to supporting us long-term as we grow and expand.
In 2023 we aim to treat 2,800 people and in 2024 we aim to treat at least 6,000 people throughout Ecuador. We believe that this will be possible based on our experience in launching the pilot: while we only have 50 spaces available this fall, we received over 200 registrations, demonstrating that there is a significant demand for our services. Furthermore, our goals for scaling are achievable as one community facilitator can be trained for only $193, and can reach 420 people each year. By the end of 2024, we plan to have at least 50 certified facilitators.
Our plan for the next two years is to solidify the model working in Ecuador, and then quickly move to expand to other high-need locations within Latin America. The overarching five-year vision of Vida Plena is to be recognized as the mental health leader in Latin America - in both quality of treatment and reach.
With the support of Samuel Dupret, a researcher with the Happier Lives Institute, we have put together a predictive cost-effective analysis for Vida Plena, in which we estimate it will cost $17 to improve a recipient’s wellbeing by one wellbeing-adjusted life year (WELLBY). For a comparison, this is 8 times more cost-effective than GiveDirectly (a gold standard charity which delivers cash transfers in low- and middle-income countries).
Co-founder team:
| Anita Käslin Clinical psychologist who secretly loves animals more than people
|
| Joy Bittner Masters in nonprofit management & aspiring runner
|
Conclusion: If you care about improving global mental health, here’s how you can help:
- Tell others in your network about us: the best connections are unexpected -we are looking to connect with people and organizations involved in global mental health, both in industry and academia. Stay in touch so we can keep you up to date with our work, sign up here.
- We’re also on instagram: @vidaplena.global
- We’re also on instagram: @vidaplena.global
- Support us financially: we plan to treat 2,800 people in 2023 and 8,700 in 2024, but have yet to secure the full funding to do so -still, every $77 provides treatment for one person, bringing us that much closer to that goal
- In total, we are looking to raise $64,000 by the end of 2023
- Thank you for donating here or you can email us at joy@vidaplena.global
End note:
I’ve been extremely nervous to write this post, feeling a bit like I'm sending out the birth announcement for my new baby, and worried you might find her wrinkled and pudgy. But like any new parent, I am also extremely proud of how far we’ve come in such a short amount of time. So, in honor of the spirit of the season, I want to say how incredibly grateful I am to all the people who have listened to my excited ramblings and said “yes, let’s make this happen.”
I could never thank enough each of you who have inspired and guided me, but still, here is a very basic attempt:
I feel especially thankful to the team at the Happier Lives Institute - for letting me work for them half time, while getting this off the ground, and not complaining when I had to leave them. This is the short list of all they have done for me. The long list is very long indeed.
So much thanks to Charity Entrepreneurship for the uncountable hours of learning and for all the doors you have kicked open for me (...even though you rejected my application the first year I applied - which taught me adversity teaches resilience, and besides, you rejected me in a way that still said, we believe in you…it's just no one funds mental health. And then the next year you found the few people who fund mental health. And you continue to kick down doors.)
Also to my fellow CE incubatees this year and all past years. I love this pack of wild people who “get shit done.” You leave such big footsteps to follow in.
Thank you so much to everyone on my board of directors, and everyone else who has given me so much of their time for free - mentoring and coaching me, proofreading proposals, building our website, sharing contacts, sharing tips and advice, a listening ear, and so much love.
Thank you to everyone who has given financially. For taking a risk when I had nothing more than an idea on (digital) paper. I would still be working for HLI increasing happiness if it wasn't for you.
Thank you to CEA, for all they do in organizing every EAGlobal, allowing me to meet so many incredible people. The virtual world is wonderful, but there’s a reason we all get on a plane to eat dinner at the same table whenever we can. Thanks for setting that table with so much vegan food.
To all my EA friends who have lent me a couch, discussed the deeper things in life, or joined me in a dance party. You are the biggest unexpected blessing I have found along this wild journey.
Thank you, especially to Samuel Dupret for sacrificing his own mental health writing and patiently rewriting the predictive CEA when I changed the predictive numbers, yet again.
And thank you to everyone in Ecuador, who is there doing the backbreaking daily work on the ground. Especially for my dear co-founder, Anita, who dared to say ‘yes’ when I asked her to jump off this blind cliff together.
And finally, thank you, dear reader, for coming along all the way here to the end of this post. I am so grateful for this community of people, who in the face of so many opportunities to fall into bitter despair, still desperately hold on to the crazy optimism that this tattered world can in fact be made better, and that it is within our power to do so. Carry on, carry on.



This is so great to see, both the intervention, progress to date, and your future plans. The post was very engaging to read as well. Thank you for this, Joy & Anita!
Thank you so much, Judith! I am so deeply grateful for all that CE has been for me personally and Vida Plena!
Congrats on the launch!
Curious about how it scales, does the training of facilitators take place always in person, I could imagine over 100 hours is quite a long time to spend to get new recruits up and going, and would they be able to attend it if they are from a remote area etc?
Hi Simon, thanks for your questions and you bring up good points!
For the facilitator training hours, it was a mix of in-person and virtual:
- 2 days of orientation in person
- 4 days of interpersonal therapy training. We had the group gather in-person, but the training was actually led virtually by a team from Columbia University. So potentially in the future, people who are unable to attend in person could attend virtually only
- the remainder of the training hours occurred during weekly supervision meetings which happens fully virtually
Our plan for future trainings is to hold them in cohort groups of people who are all from a specific geographic region, so we could just send the trainers for the duration of the training days.
Alternatively for cohorts groups who are more disperse, we will likely have to help with the public transportation costs, but we have a partnership with a local conference center who has promised to house us for free.
In general, this is a we have budgeted for a 30% turnover rate for our facilitators each year.
Happy to share the training budget details with anyone who is interested: joy@vidaplena.global
This probably isn't something you want to spend a ton of time right now thinking or writing about, but I am curious about the medium/long-run funding model you have in mind. Specifically, I am wondering if you thought it would be viable in the medium to long run to obtain a significant fraction of needed funds through small payments by clients, in-country fundraising, and/or partial government support. (That is not a suggestion that you should be trying to raise money from these sources in the near term!)
Among other reasons I am excited to see VP launch, I am interested in having the community gain knowledge about how an EA organization might be able to capitalize on the advantages of being in a medium-income country as opposed to a low-income one. For instance, in my decision to make a small donation to VP in 2023, I gave moderately significant weight to the leadership team coming from outside a high-income country. Nothing against people from high-income countries (of whom I am one), but I think your operating model could potentially open doors to certain non-EA donors who strongly preference organizations that are closer to the communities they serve. For instance, I think that the team collectively having been on the ground for decades prior to starting operations could be a strong selling point for donors in many Christian communities.
I do suspect the CEA is on the optimistic side based on the concerns that have been raised about StrongMinds' own CEA, and the assumption that work in a high-medium income country will be less cost-effective than in Uganda. So one of the ideas I'd be interested in seeing VP consider (at the right time!) is whether it can use EA dollars for startup/development and then as partial funding to leverage/multiply in-country resources, rather than having ongoing operations nearly-100% funded by Western donors. That kind of leverage strikes me as a potential way to make donations to work in middle-income countries have cost-effectiveness profiles closer to those we see for work in low-income countries.
The other question/observation I have about work in a medium-income country is whether the ability to eventually raise some fraction of money in-country could be a useful signal that the community values the work the non-profit is doing. While I don't agree with most critiques of global health/development charities as Western imperialists, I think I would consider evidence of local buy-in when evaluating a charity in a middle-income country that is more than a few years old. In contrast, I would assume that the reason the low-income country charity doesn't have measureable local buy-in is unrelated to the community's interest in the charity, but wouldn't automatically make that assumption for a developed charity in a middle-income country. Of course, there are other evidences of local buy-in, such as an extensive volunteer network, so I don't mean to privilege funding over other forms of evidence.
Hi Jason! Thank you so much for all your very thoughtful comments and ideas! (and also for your decision to support us in 2023!) Want to take a minute to respond to some of your points:
Funding from non-EA sources: absolutely! We are so grateful that the EA-community is willing to take some risks on new organizations before they have a track record. With the results that we are able to demonstrate early on, we are absolutely planning on applying for counterfactual funding. In fact, as an example of this we were just selected to be part of the South Park Commons Social Innovators Fellowship, which is hosted in collaboration with the Agency Fund.
Mixed-payer model / sliding fee scale: yes, this is also a possibility we are keeping in the cards if needed, always keep in mind our mission. Our target populations are low-income communities and refugees: people who would not otherwise be able to access services (for example, we've found for some people even the $0.50 bus fees to attend are prohibitive). Additionally, I have talked with other mental health program founders (from Europe) who have warned me of being careful about the mission drift that can happen when taking on high-value paying customers (even with the positive goal of them subsidising other people...seems even with the best of intentions, they say it can be hard not to end up focusing more on the people who pay...).
Local fundraising / government funding: yes! This is actually part of our long-term plans. There is significant research that demonstrates improving one's mental health results in improvements to physical health. We would like to demonstrate that this program can actually be a cost-savings to the national public health system. Furthermore, a recent UNICEF study found that untreated mental illness costs $30B a year in Latin America, making a very good case for national governments to dedicate more of their current public health budgets to mental health (currently less than 2% according to the PAHO).
Local leadership and talent: I completely agree, - this is one of my favorite points that you bring up! Latin America is full of highly educated, very experienced professionals, and so this is who we will continue to hire. Something that differentiates us from Strong Minds. I am committed that our staff from all levels be locally based in Latin America, both as a cost-savings measure and especially to benefit from this incredible local talent- their professional connections, local knowledge, and personal understanding of the needs of the people we serve.
Happy to chat with you further or answer any other questions that might come up - open invite to anyone to find a time on my calendar.