Niek Versteegde, founder GOAL 3
Posts 1
Comments8
Hi Ian,
Sorry for a delayed response. But indeed you are right abou this. However, the costs at the hospital staff for availing staff is actually very low. Typically it is 20-30 people for 1 day, the costs are negligible in relation to the 10 year total costs. Moreover in-service training is part and parcel of every nurses job and part of the hospitals responsibilities. That is why we have not counted it so far.
In the coming months we expect to have a proper assessment of the impact on workload and costs and can more clearly describe it as a benefit. Initial results from one hospital indicate that IMPALA is leading to a significant cost-reduction. Will keep you posted about developments.
I guess then it's just my title: In God we trust, but all others must bring data. It just feels frustrating sometimes, also because people actually don't say they don't believe you. So if you don't call me a liar, then why don't you help or support me?
I would really like it if a more systematic way of identifying, testing and scaling successful innovations was available.
My post are definitely not intended to complain by the way. I am blessed with a great and supportive team and have great partners as well. It's a genuine interest to understand, learn and improve.
Hi Ian (and John),
Actually we think these are all costs. To clarify a bit: we are operating as a social enterprise. The prices mentioned here would be what the hospital/NGO/government pays. Implementation is done with local staff which is quite affordable, after implementation everything is done by hospital staff. There is only limited need for support and maintenance which is all done by local teams which keeps costs low. Because (assuming we will reach sufficient volume) there are margins on the product and services this will ultimately pay for all international staff including mine.
Hospital staff time/costs goes down after the intervention, because the system automates repetitive tasks. Moreover we see a 10% shorter admission time, which will also have a positive impact on workload.
Soon we will publish more results showing that both costs for the health system and the patient will go down after the intervention. Based on what we see so far it is even very likely that our intervention is net cost saving over time.
We didn't include that in this analysis because we did not yet have the results and it again complicates it further.
Dear John,
Thanks a lot for your candid feedback. This is exactly what I hoped to get from this forum.
Honestly speaking it has been quite a struggle to think what could be the right tone and what information should be included and what not. What we do is not that simple and the context in which we operate isn't either. I guess you have captured my failure to strike the right balance well with your feedback.
What might help to better understand what we do is our product video. I didn't include it before because I don't want people to feel like I am here to promote my work. Curious if you feel it should be included.
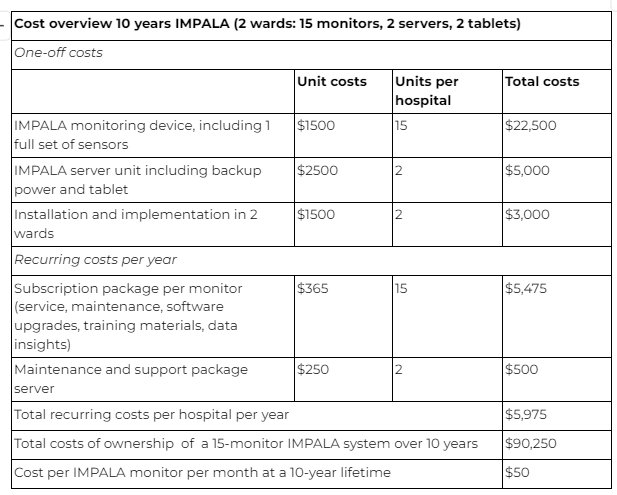
Regarding the costs remark, actually everything is included in the costs that we presented here. You can find a detailed breakdown with rationale at the bottom of this document from which I took the screenshot below. If we can achieve sufficient scale (>5000 devices) we can deliver and sustain it at the costs presented below and likely for sifnificantly less if we achieve a bigger scale.
Unfortunately I do not have time to rewrite and organize everything right now, but hopefully I can make some improvements over the weekend. If you are open to it, I would gladly receive your feedback before updating the post.
Hi Ian, thank you for your thoughtful feedback. We fully agree that independent evaluations and randomized controlled trials (RCTs) are an important tools for understanding impact. However, we must also acknowledge that RCTs come with significant costs, long timelines, and often produce results that don’t fully translate into real-world settings. Our experience has shown that the complexity of low-resource healthcare environments requires adaptable, on-the-ground solutions that are continuously tested and refined in real-time.
That’s why, at GOAL 3, continuous evaluation and learning are embedded into our approach, aimed at Real World Evidence. We feel that waiting for a one-off trial to tell us whether IMPALA works is not appropriate. Instead, we are committed to assessing our effectiveness at every site in the real-world, following up over time, and ensuring year-on-year improvement. This approach allows us to make iterative and localized changes based on the needs of health workers and patients, ensuring we create a sustainable impact that lasts. Our goal is to see a measurable improvement not just immediately after implementation but as a consistent part of the health system's development.
Of course we do want this to be evaluated independently, to also assess unanticipated negative and/or positive impact from the intervention. We know we are biased and we understand that we are not the best evaluators. That is why we leverage the Founders Pledge grant to ensure independent research institutes can do this evaluation across different settings. This will strenthen the evidence on effectiveness across different settings with a larger poule (7) hospitals, over time (>1year follow-up) while also assessing differences.
On a personal note, while I understand and endorse the rigorous processes that donors and evaluators require, I sometimes feel frustrated by the lack of urgency. The slowness of decision-making in global health is an enormous barrier to innovation. Many life-saving solutions are delayed because innovators and startups simply don’t have the time or resources to wait for trial results. During COVID-19, we saw how innovations were fast-tracked to address an urgent crisis. It feels unfair that the 5 million pediatric deaths every year are not considered urgent enough to prioritize similarly fast solutions. Basically the risk of unanticipated consequences should be balanced against the potential positive impact and use that to navigate decisions about
Ultimately I agree with the process and I should not complain after receiving a grant from Founders Pledge to support us in building the evidence base that is needed. Its just that I am frustrated because it feels like a continuous fight to move things forward or even survive, while deep in my heart I know we are right and that every delay will hinder us from preventing deaths that are unneeded.

Hi Toby,
Apologies for a belated response. You are correct that there are quite large seasonal influences. So we matched everything with the respective months in the same period to compensate for it. 2 weeks ago we also got the individual patient level data. This data shows that the post-intervention group was actually on average in a worse condition than the pre-intervention group. If this is taking into account the mortality reduction is close to 50%.
Regards,
Niek