How this report is having an impact This report is a shallow dive into life in slums, which is a sub-area within global development. This report was produced as part of the Cause Innovation Bootcamp and reflects approximately 40-50 hours of research, offer a brief dive into whether we think a particular problem area is a promising area for either funders or founders to be working in. Being a shallow report, should be used to decide whether or not more research and work into a particular problem area should be prioritised. |
In a nutshell
|
Key uncertainties
|
Author: Taylor Sweeney Editors: Akhil Bansal, Leonie Falk |
Table of contents
1. Is this cause area important?
a. Health in slums
b. Why are slums so unhealthy? An introduction to neighbourhood effects
c. Infectious disease
d. Nutrition
e. Other measures of health
f. Slum data deficits
g. Geographic distribution of the problem
a. Slum policy interventions
b. Resettlement
c. Legal recognition
d. Security of tenure
e. Slum health as a discipline of study
f. In situ slum upgrading interventions
g. Water and sanitation
h. Home improvement
i. Lighting, repaving, garbage removal
j. Community engagement: a vital framework for conducting interventions
a. Why aren’t non-profits funding urban slums?
b. Organisations
4. Conclusion
5. Footnotes
6. References
Is this cause area important?
Approximately 1 billion people live in slums across the world, and this is projected to double before 2030, accounting for one quarter of the world population. Slums are described as “contiguous settlement[s] where the inhabitants are characterised as having inadequate housing and basic services” (UN-HABITAT, 2003). Slum populations are uniquely disadvantaged by problems including insecurity of land tenure, densely-populated and often geographically dangerous land area, and poor living conditions which act as vectors for disease. Slum dwellers consistently score lower than comparable rural or non-slum urban populations across myriad health outcomes.
Where there came urbanisation, so too did slums. The word ‘slum’ was first coined in the 1820s, used to describe areas of London with particularly low quality housing and hygiene. Today, the United Nations classifies slums by five criteria:
- Lack of access to improved water source
- Lack of access to improved sanitation facilities
- Lack of sufficient living area
- Lack of housing durability
- Lock of security of tenure
Ever since the Industrial Revolution, people have been drawn to urban areas at a rapid pace to meet demand for the production of goods. Informal settlements were viewed by many as an upgrade on the monotony and poor conditions of rural life. Slums became ubiquitous first in the developed world, then, particularly in the 1980s and 90s, became more prevalent in developing nations as the demand for cheap labour rose. While building and hygiene regulations have mostly eliminated slums in high income countries today, slums continue to grow in low and middle income countries (LMICs). As three million people globally move from rural to urban areas every week, slums are set to house 2 billion people, or a quarter of the world’s projected population, by 2030 (Ezeh et al., 2016; UN Habitat, 2020). The perception that slums are a transition point between rural poverty and the urban middle class must therefore change. Many now call slums their permanent home. As a result, the health of their populations require careful analysis and targeted interventions.
Health in slums
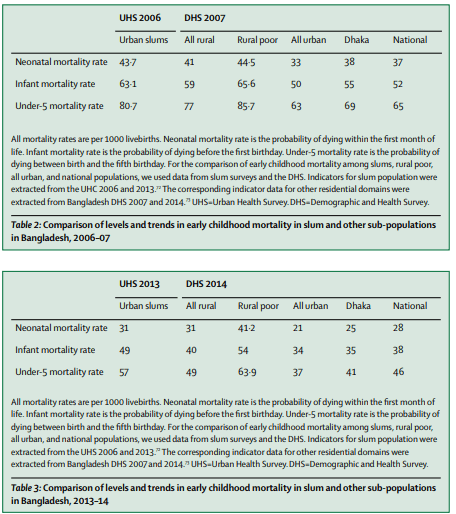
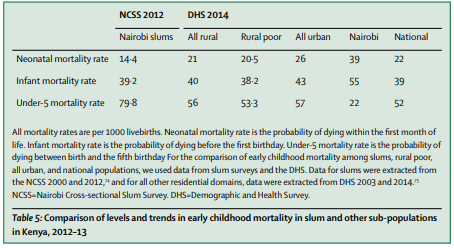
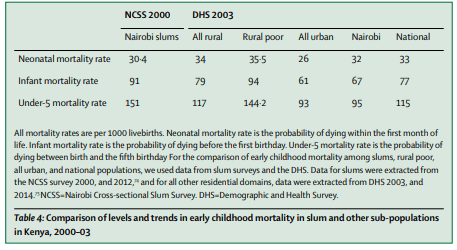
The health of slum dwellers is significantly worse than non-slum populations. Since slum dwellers move often and sometimes move rurally to die, life expectancy is difficult to estimate. This leaves child mortality as the best ‘broad-brush’ health measure. Higher infant and neonatal mortality has been reported in slums than rural areas across Kenya, Ecuador, Brazil, Haiti, and the Philippines. Further stratification of Bangladeshi and Kenyan populations reveals child mortality in slums to be worse than urban, rural, and rural poor populations (see Figure 1). In fact, child mortality in Bangladeshi and Kenyan slums, on average, is 33% higher than the national average, and even 7% higher than in poor rural populations. As such, health in slums can no longer be accepted as an improvement on the rural poverty many slum dwellers are seeking to escape. Indeed, slum health is worse than rural poverty.
Why are slums so unhealthy? An introduction to neighbourhood effects
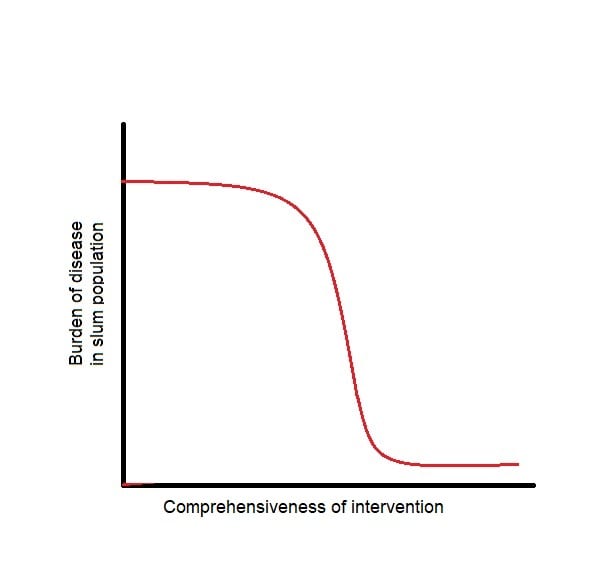
Living in a slum and living in poverty (even in an urban, non-slum context) does not produce the same health outcomes. The health of slum dwellers is largely dictated by environmental risks, such as contaminated water supply or poor housing quality. High population density means such risks are usually shared by everyone in the slum. This phenomenon is referred to in the literature as “neighbourhood effects” and is not observed in either poor rural or urban non-slum populations (Ezeh et al., 2016). Acknowledging neighbourhood effects is important for a few reasons. First, it means that interventions which lack comprehensiveness or try to intervene at the individual/household level often fail to deliver desired outcomes - this is a theme throughout the Interventions section of this report. Conversely, it means slum dwellers will often benefit collectively from comprehensive interventions. It is hypothesised that as a slum intervention becomes more comprehensive, health outcomes will improve exponentially.
Infectious disease
Slums have a very high burden of infectious disease. Diarrheal disease is particularly prevalent in slums, resulting from bacterial contamination of water supply, and disproportionately affects children under 5 years of age. In Egypt and Kenyan slums, childhood diarrheal disease is, on average 29.5% more prevalent in slums than the national average (Kenya: 20.2 vs 15.2 per 1000, Egypt: 23.9 vs 18.9 per 1000) (Mberu et al., 2016). In India, fever is 63% more prevalent in slums than non-slum areas (9.8 vs 6.0 per 1000) and diarrheal disease is 45% more prevalent in slums than non-slum areas (6.8 vs 4.7 per 1000) (Mberu et al., 2016).
Slums also act as the perfect breeding ground for vector-borne and zoonotic diseases (VBZDs). For example, leptospirosis, a viral infection carried by rats, disproportionately affects slums because rat abundance is closely associated with human density, open sewers and sources of food - all conditions fulfilled by slums (Costa et al., 2017). While most infectious diseases worldwide are becoming associated with less mortality and morbidity due to vaccination, Zika virus and dengue fever are both increasing in this regard. These two diseases are vectors of the Aedes aegypti mosquito, which breeds in shady, dirty water often found in containers or puddles. While data is lacking, the burden of Zika and dengue are hypothesised to be higher in slum populations as a result (Costa et al., 2017). In contrast, slums provide protection against one vector-borne disease: malaria. Its vector mosquito, Anopheles, prefers clean, sunlit water surrounded by vegetation, which is not typically found in slums.
Nutrition
Under-nutrition is the leading risk factor for disease burden in sub-Saharan Africa. Across three systematic reviews, slum dwellers have been identified as nutritionally disadvantaged compared to their urban non-slum counterparts (Ezeh et al., 2016). Under-nutrition is associated with recurrent diarrhoea and consequent growth stunting, which is also more prevalent in slums than non-slum urban, rural and national contexts in multiple regions. Breastfeeding is known to reduce incidence of diarrhoea and pneumonia, as well as reducing all-cause mortality in LMICs. However, breastfeeding rates are low in slums, likely due to labour market demands prohibiting women from staying home or taking their babies to work with them (Ezeh et al., 2016).
Other measures of health
Mental health and rates of non-communicable diseases (NCDs) arguably carry a higher burden of disease than communicable diseases in LMICs today. However, literature on slum mental health and NCDs is sorely lacking. This report identified one systematic review which indicated that children in slums faced a higher burden of emotional and behavioural disorders than those living in urban non-slum or rural areas (Ernst et al., 2013). In relation to NCDs, childhood asthma is more prevalent in slums, while hypertension rates are slightly lower in slums (Ezeh et al., 2016). Beyond this, little data has been identified by this report on the prevalence of other major NCDs.
Slum data deficits
Slum health is an understudied area. The root of the problem lies in the way census data for slums is collected. Demographics and Health Surveys (DHS), which are used as censuses in many LMICs, do not distinguish between households in urban slum and non-slum areas. Furthermore, there are many technical difficulties in counting slum populations - slum homeowners are often absent, households are not on defined blocks of land, and census staff can be afraid to enter slums. This lack of census data makes it difficult to study slum populations and understand their demographics and health measures, and tailor interventions accordingly.
Even using the available data, academic research into slums is lacking. Ezeh et al. (2016) found that only 2.8% of LMIC studies on MEDLINE and Embase which stated their location were based in slums. A mere 7% of WHO Clinical Trials which stated location were conducted in slums, and many simply used slums as a convenient location to study a topic other than slum health. This results in a small sample size for slum health and wellbeing findings, which increases the risk of bias.
Geographic distribution of the problem
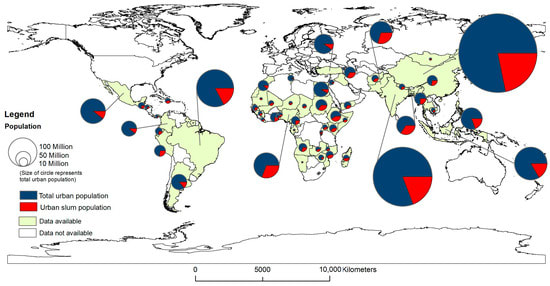
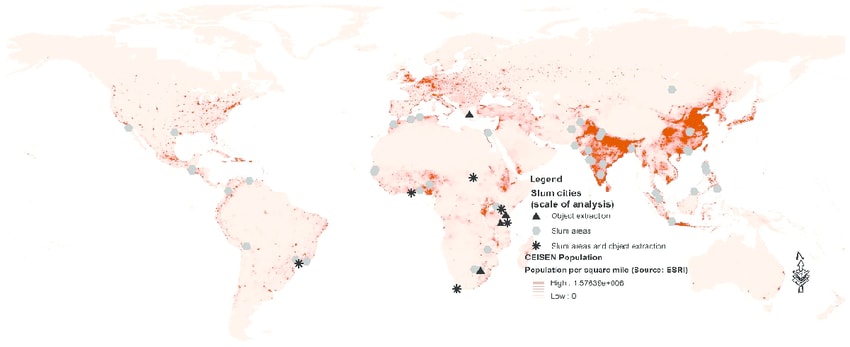
Slums are a worldwide problem, but are particularly prevalent in low to middle income countries where urbanisation occurred quickly. The World Bank (2018) reports countries with the highest percentage of total population living in slums to be across Africa, South Asia and South America. This is evident in Figure 2 and 3. India and China have the largest population of slum dwellers, while countries in Central Africa have the highest percentage of their urban populations living in slums (Mahabir et al., 2018).
Most slums occupy a similar land area. Friesen et al. (2018) found that 84% of slums in eight cities across South America, Asia and Africa occupy a land area of 0.001 to 0.1 km2. There is no strong correlation between region and slum unit size, however, South America cities tend to have larger slums, while Asian cities tend to have a number of smaller slums.
Tractability/Interventions
There are two types of interventions that address the problems of slums, policy interventions and in situ slum upgrading projects.
Intervention | Does it work? | Who funds it? |
| Slum policy | ||
| Resettlement | Unlikely | Government |
| Local governance | Unlikely | Government |
| Security of tenure | Unlikely | Government |
| Slum research | Promising | NGO, UN, academia |
| In situ slum upgrading | ||
| Water and sanitation | Yes | Gov, NGO, UN (NGOs: WaterAid) |
| Home improvement | Yes | Gov, NGO, UN |
| Lighting, repaving, garbage removal | No / not enough data | Government |
Slum policy interventions
Resettlement
Resettlement programs for slum dwellers have largely failed. Remember, many people choose to move to slums because of their proximity to work and, for many, a better life than could be had if they continued to live rurally. Relocation programs move slum dwellers into government housing, either to improve living conditions or re-develop the slum land. Across a variety of contexts, slum resettlement programs have worsened living conditions for slum dwellers, even when the project aimed to improve conditions (Kapse et al., 2012). New housing is usually further away from industry, so resettled populations report less job opportunities and longer, costlier commutes. Government housing often charges rent, which resettled individuals cannot afford. Resettlement programs have also failed to deliver promised infrastructure. These factors result in many moving back to their original slum or even forming a new slum, often with even worse living conditions.
Resettlement also appears an unsustainable policy because rural to urban migration is expected to increase over the next decade, so slum growth will likely outpace any resettlement program. While a well-designed city expansion project coupled with resettlement of slum dwellers into permanent housing may ameliorate many issues faced in slums, the cost of such a program is far out of the reach of most LMIC, especially considering the slum dwellers will be unable to pay much/any rent.
ToC
Inputs: Relocate slum dwellers into government housing commissions at a small rental rate
Outputs: security of tenure, improved water and sanitation, access to government services, reduced environmental risks
Outcomes: Better health outcomes inc. child mortality/morbidity, alleviation of poverty traps
Impact: Improved subjective wellbeing, Government use slum land for another purpose
BOTEC
Not required as this intervention has a null to negative impact.
Legal recognition
Many slums are not even recognised on maps or zoned by cities, often as a political move to avoid providing municipal services. Over 20 years, Nolan et al. (2018) found that living conditions in legally recognised slums progressively improve the longer they are legalised for, compared to non-legally recognised slums. Most Indian states recognise a slum’s existence based on length of residence.
Currently, no organisation that could be identified in this shallow report is fighting for legal recognition of slum areas. An NGO could feasibly lobby governments like India to loosen slum recognition criteria or disentangle the provision of basic services with slum recognition. Tractability of this intervention would largely depend on the political will for such an intervention, something I am very uncertain of and would likely be very heterogeneous, even within countries.
ToC
Inputs: convince governments to loosen slum legalisation criteria
Output: more legalised slums
Outcomes: slums have access to government services
Impact: improved health outcomes via water and sanitation upgrades
BOTEC
This BOTEC includes a high degree of uncertainty. In India, political lobbying is considered corruption. This leaves political activism, an intervention with high costs and low probability of success, considering political motivation to legalise more slums is low (this costs governments more money). While I have not produced a quantitative BOTEC for this intervention, I highly doubt it would be cost-effective due to the low chance of success.
Security of tenure
Many slums are informal settlements where residents do not have tenure over their land. Evidence suggests providing security of tenure leads to increased investment into home improvement and sanitation. In a natural experiment in Peru, landowners awarded title invested almost twice as much as the control into their homes, without requiring more credit (Field, 2005). Again, research into the existence, extent or cost of such a program is lacking.
ToC
Input: provide security of tenure to slum dwellers
Output: increased investment into homes
Outcomes: better sanitation and shelter quality
Impact: reduced waterborne disease, increased subjective well being
BOTEC
Similar to previous interventions, this BOTEC includes a high degree of uncertainty, as there is no clear path to advocating for security of tenure. This must be through the government, who in many developing countries, do not look kindly towards political lobbying. This is consistent with research – security of tenure has not been evaluated in an RCT simply because security of tenure can only be provided by a government, not a research group. Therefore, this intervention has been labelled ineffective on the grounds that it is intractable.
Slum health as a discipline of study
Research into slum health is sorely lacking in two key areas. First, health data for slum populations is insufficient. When census data for slum populations is available, it is usually lumped together with non-slum urban populations. Burden of different diseases is poorly studied in slums; for example, dengue fever and Zika virus prevalence has seldom been compared between urban slum and non-slum populations, so we do not know if prevalence is actually higher in slums. This is a problem because, as identified earlier in the report, living in a slum and living in poverty does not produce the same health outcomes.
This leads me to my second point: we do not fully understand neighbourhood effects, a phenomenon which uniquely affects the health of slum dwellers. It is hypothesised that a dose-response curve for a slum upgrading intervention and associated burden of disease would look something like Figure 4. To investigate this, an RCT would be required which performs an intervention with varying degrees of comprehensiveness at different sites, e.g. a sanitation system which covers every home vs 50% of homes vs 25% of homes vs control. This would provide important data on how comprehensive an intervention needs to be to deliver cost-effective results in a slum population. Better understanding of the problems facing slum populations would allow for more targeted and cost-effective interventions going forward.
ToC
Input: more research into slum health
Output: better understanding of factors dictating slum health
Outcome: more targeted and cost-effective slum health interventions
Impact: better subjective wellbeing and health outcomes for slum dwellers
BOTEC
A BOTEC for this intervention includes a high degree of uncertainty because RCTs vary widely in cost and efficacy depending on the usefulness of research, which is difficult to predict.
This report failed to identify any systematic reviews which estimated the cost of an RCT in development economics. The Abdul Latif Jameel Poverty Action Lab (J-PAL), a key actor in the field of development economics, is estimated to have received $300 million in funding between 2003 - 2018, in which time they conducted 876 RCT’s. By this estimate, an average development economics RCT costs $342 000, including the costs of running an institution almost entirely dedicated to producing RCTs.
Cost-effectiveness of research is near-impossible to estimate because the margins for error are so large. For example, let’s say one RCT halved the cost of delivering piped water interventions in slums. Piped water currently costs $206 per household, and there are roughly 182 million slum households globally. If this intervention was applied to every household, conducting the RCT would save funders $103 per household - that’s $18.7 billion saved directly through this RCT, to achieve the same amount of DALYs (0.86 per household or 157 million globally). This makes the $342k per RCT look like a rounding error. Conversely, the RCT could fail to save any lives or costs, making it $342k wasted.
Therefore, slum research is a promising intervention with great potential to fuel better interventions for slums, but also carries a high risk of failure.
In situ slum upgrading interventions
Water and sanitation
Piped water and adequate sanitation facilities are likely highly cost-effective interventions in slum environments, but evidence is limited. Evidence for the provision of safe drinking water is well-established in non-slum contexts, so theoretically, improving water and sanitation in slum contexts should prove even more effective due to neighbourhood effects. A Cochrane systematic review identified one study which found a significant reduction in diarrhoeal disease incidence and duration in slum households receiving piped water compared to a control. Participants also saved 4.5% of their annual income by eliminating the cost of bottled water. A multi-component intervention study involving installing piped water and lavatories in homes, whilst paving streets and installing drainage systems resulted in a 61% relative reduction in waterborne diseases. Beyond these two studies however, results have largely been disappointing. One sanitation intervention RCT showed no effect on mortality, but other studies not specific to slums have shown significant reductions in diarrhoeal disease incidence resulting from improved sanitation. A plausible explanation for such results is that the smaller scale of these quoted studies fails to take advantage of neighbourhood effects in slums. It remains unproven whether water and sanitation interventions delivered concurrently have greater effect than independently.
ToC
Clean drinking water
Input: Provide piped water taps
Output: Slum dwellers have access to clean water
Outcome: reduction in diarrhoeal disease
Impact: better health outcomes, improved subjective wellbeing
Sanitation upgrading
Input: provide flush/septic toilets
Output: Separation of human faeces from food, water and contact
Outcome: reduction in diarrheal disease
Impact: better health outcomes, improved subjective well being
BOTEC
Access to piped water causes an absolute risk reduction of diarrhoeal disease incidence of 0.1047. Average duration is also reduced by 84%, so let’s say absolute risk reduction of 0.1047 x 1.87 = 0.1926, considering both incidence and duration (Galiani et al., 2009). Diarrheal disease causes 0.81 DALY per incidence. Therefore, piped water adds 0.156 DALY per person, or 0.858 DALY per household (assuming 5.5 people per slum household on average).
Reductions in water cost resulted in a 4.5% increase to annual family income. If we assume people value one year of healthy life at 2.5x their annual income, we get 1 x annual income = 0.36 DALY. Therefore, savings from piped water results in 0.016 DALY per household.
I am highly uncertain about the cost of this intervention. Generally, the cost of installing household water connections is $148 - $258 (Hutton & Bartram, 2008). However, the intervention studied involved a private company which would waive the cost of installation if the community provided labour. The company would charge for raw materials and training of labourers, then charge a $1.7 fee per household per month.
At typical costs, this intervention results in a BCR of $169 - $295 per DALY.
However, this cost could be significantly reduced through the use of community labour and intelligent policy making. Community engagement policies could be integrated to improve participation, and thus cost-effectiveness. This intervention is highly cost effective.
Home improvement
Building better houses in slums seems to relieve some of the disease burden and poor quality of life associated with shanty houses. Galiani (2016) evaluated the efficacy of an NGO called TECHO, which provides small, prefabricated houses to families living in Latin American slums. 20-40% increases in subjective quality of life are reported, but these gains dissipate within two to three years due to hedonic adaptation. Incidence of childhood diarrhoeal disease (CDD) is reduced by 18% in treatment households, while incidence of respiratory disease is not affected. This is significantly higher than the 2.7% risk reduction for CDD reported in a Mexican natural experiment providing cement floors in slums. It remains unclear whether this divergence is due to the difference in intervention (floors vs houses) or accuracy of experimentation.
ToC
Input: provide prefabricated houses or cement floors to slum dwellers
Output: better household cleanliness and livability, as houses provide security, dryer and more temperate environments, safer storage of food and belongings
Outcome: reduced diarrheal disease in children
Impact: improved subjective wellbeing and lifespan
BOTEC
One cement floor costs $150 USD (Maclay, 2009). Anaemia causes 0.027 DALYs per incidence, while diarrhoeal disease causes 0.81 DALYs per incidence (IHME, 2022a, 2022b). Cement floors caused an absolute risk reduction of 0.083 for anaemia and 0.018 for diarrhoea (Titiunik et al., 2007)
Therefore, cement floors cause 0.015 DALY / child via diarrhoea reduction and 0.0022 DALY / child via anaemia reduction (total 0.017 DALY / child).
Slum households on average house 3.5 children, so one cement floor will cause 0.060 DALY / household via child health improvements.
This equates to $2485 USD / DALY.
This BOTEC is likely to underestimate the CBR of cement floors because I have only considered childhood diarrhoea and anaemia prevalence, not improvements to adult health, other child health measures, or wellbeing benefits.
Note: a BOTEC has not been completed for entire houses (only cement floors) because each house costs $24 000 and achieves only slightly better child health outcomes and improved mental health (World Habitat, 2015). Despite this, the high cost means the CBR will likely be much lower than for cement floors. Having said that, there might be cheaper ways to add to the quality of existing houses (e.g. roofing material, floors) and cheaper ways to build houses but for this to be cost effective a house would have to be at least ten times cheaper (~$2400).
Lighting, repaving, garbage removal
Slums commonly lack basic urban services and infrastructure; the most pertinent of these being street lighting, paved streets, and garbage removal services. Unfortunately, few experiments have been completed assessing the effects of providing such services. Gonzalez-Navarro and Quintana-Domeque (2016) provided paved streets in a Mexico slum, finding a 109% return on investment in property values, and increased rates of home improvement and consumption. Consumption increases are hypothetically related to the wealth effect: with more wealth (via property value), people feel more comfortable buying more. No health outcomes were measured. A single RCT improving lighting demonstrated a null effect, while garbage removal services have not been adequately studied to evaluate efficacy.
ToC
Input: urban infrastructure or absent municipal service
Output: increased property value
Outcome: build wealth of slum dwellers, encourage investment into home improvement
Impact: positive cycle of improved slum infrastructure, improve wellbeing
BOTEC
Paving streets in this study cost $701 per land block on affected streets and generated $796.8 of value per block. In Mexico, annual income at the relative urban poverty line is $20 496. Assuming one person per land block, paving streets adds 0.039 x annual income in land value. Assuming 1 x annual income = 0.36 DALY, this intervention results in 0.014 DALY per land block. This equates to $50 071 per DALY. Therefore, this intervention has negligible impact.
This likely underestimates DALYs as it fails to consider health outcomes or long-term income gains resulting from better access to employment locations. While unappealing to NGOs, this intervention may appeal to governments as it offers a marginal benefit to citizens whilst likely recouping construction costs in the long-term through land tax increases resulting from increased property value.
Community engagement: a vital framework for conducting interventions
A growing literature indicates that community engagement in an intervention may multiply its effects (Lilford et al., 2017). A systematic review finds greater behavioural outcome effect sizes resulting when the community is engaged throughout the design, implementation and evaluation of an intervention (Lilford et al., 2017). This is likely due to increased participation in the intervention, but may also be due to the intervention better meeting the community’s needs (Brunton et al., 2015). Failure to engage with the community may conversely result in intervention failure; for example, two recent RCTs in India assessing pit latrines failed simply because people chose not to use the facilities. Therefore, it is important that slum communities are engaged throughout any intervention to improve its outcomes.
Neglectedness
Most funding for slum upgrades and slum policy comes from states. The UN and NGOs provide support to low income countries or politically unstable countries who are failing to provide services to slum dwellers (UN-Habitat, 2022). However, a recent economic report suggests slums require global investment of US$6.5 trillion to achieve urbanisation benchmarks outlined in the UN Sustainable Development Goals by 2030 (Global Steering Group for Impact Investment, 2022). This is more than four times the current level of investment in developing-world infrastructure projects (UN-Habitat, 2022). UN-Habitat, which funds slum interventions among other urban planning projects, receives just 6% of the UN’s current budget (United Nations, 2021). Therefore, slum health appears to be a neglected cause area.
Why aren’t non-profits funding urban slums?
Historically, philanthropic funding has focused more on rural poverty than urban poverty. Non-profits are reluctant to fund urban slums due to a number of challenges - some genuine, and some perceived. When interviewed for this article, non-profit leaders cited three key reasons for this: legality, transience, and cost-ineffectiveness. First, many see slums as “illegal settlements'' and are thus reluctant to upgrade such areas in fear of legal barriers. In fact, India’s Companies Act 2013 legalises private funding for slums, and many other countries have similar legislation in place. Second, non-profits perceive slums as transient, and thus worry that slum upgrading may go to waste if the population moves. Again, this is an unfounded fear - slums are so highly-populated and rapidly growing that any mobility is highly unlikely. Finally, non-profits sometimes subscribe to the narrative that slums are unproductive and a drain on public funds. While the economic impacts of slums remain controversial, the economic benefits of slum upgrading does not. Providing better living conditions allows workers to be more productive, children to attend school at higher rates, and residents to live longer (Ezeh et al., 2016). These rebuttals suggest slums may represent an untapped resource for philanthropic funding.
Whether NGOs providing services a local government should provide remains controversial. Foreign aid improves living conditions, seems to induce economic growth, but does it also keep bad governments in power? Considering the magnitude of investment required, it seems that even well-run LMIC governments will fail to meet the needs of its slum populations. This represents an opportunity for NGOs to bridge the funding gap and deliver interventions which improve the lives and health of slum populations. However, careful consideration of the political landscape is crucial to ensuring the success of an intervention program beyond its specified outcome measures.
Organisations
Please note that these implementers have not been vetted and this is merely a quick overview about some of the implementers and is not exhaustive.
| Organisation | Annual Expenses | What they do | Geographic focus |
| Slum Dwellers International (SDI) | $14.3m | Slum-level community development, city-level slum advocacy, global slum policy advocacy | Africa, South Asia, Brazil |
| SHOFCO | $8.3m | Clean water, healthcare, education | Kenya and Bangladesh |
| Water Aid | $136 000 (total budget x 1%)1 | Water and sanitation | Developing nations |
| United Nations Human Settlement Programme (UN-Habitat) | Estimated 2022 budget: $242m | Wide variety | Global |
| Habitat for Humanity | $300 445 | Housing | Asia-Pacific |
| Cities Alliance | $13m | Advocacy / consulting | Global, concentrated in Africa |
| charity: water | $1m (total budget x 1%)1 | Clean drinking water | Africa and Asia |
Notes:
- WaterAid states that only 1% of urban development budgets reach slums. Assuming this to be true for their own organisation (likely higher), we can find their minimum slum expenses by multiplying their total budget by 1%.
Of the above charities, this report identified that only SDI had produced something similar to an impact evaluation (this study). This report could not find any specific programs which had been evaluated by an RCT, nor have any been rigorously evaluated by a charity evaluator. That said, all charities listed are transparent with their finances. SDI provides a clear theory of change and has clearly performed a level of evaluation into their programs. SHOFCO is the only of the above charities to appear on Charity Navigator, and returns a 100% score for transparency. Given this, I would provisionally recommend SDI or SHOFCO for donors interested in slum health - but individual research is required. I also recognise that until these organisations conduct an RCT on their programs, it is difficult to fairly judge their impact.
Conclusion
More research is required to determine whether slum policies could improve conditions for slum dwellers, however I doubt any policy initiative will actually be tractable. Water and sanitation upgrading appears a cost-effective intervention in slums, however most other slum upgrading interventions would likely not meet GiveWell standards. Community engagement will likely magnify the effects of any intervention. As slums grow at an alarming rate, a better understanding of problems uniquely faced by slum populations is required. For this to happen, governments must consider slums as spatial entities and collect more extensive census data, while academia may contribute by focusing research directly on slum health. Enormous investments are required just to meet UN SDG’s in slums. Despite this, only 3% of the UN’s budget is directed towards slums, and few NGOs are focusing solely or primarily on slums. Therefore, this cause area is neglected and tractable.
Overall, this shallow investigation has updated me positively on the importance of this cause area. In light of that, I recommend the following actions:
- If you are an average punter: Consider donating to SDI or SHOFCO (after conducting your own research)
- If you are a funder: Consider investing in slum-based charities based on the needs identified in this report.
- If you are a charity evaluator: Continue to consider slum-based charities as the field expands (hopefully) to meet the need.
- If you are an academic: Consider researching slum health as a branch of public health or advocating for research funding in this area in your organisation. The field of slum health could greatly benefit from RCT’s investigating neighbourhood effects.
- If you are an entrepreneur: Consider starting a charity in one of the areas of need identified within the report. Despite the need, no water- or sanitation-based charity has met GiveWell’s standards for a top charity - so an opportunity exists.
Footnotes
- Quality of life is assessed via a subjective wellbeing questionnaire provided to participants, asking “How satisfied are you with… your quality of life - Would you say you are “Unsatisfied”, “Neither Unsatisfied nor Satisfied”, “Satisfied” or “Very Satisfied”?
References
Brunton, G., Caird, J., Stokes, G., Stansfield, C., Kneale, D., Richardson, M., & Thomas, J. (2015). Review 1: Community engagement for health via coalitions, collaborations and partnerships: A systematic review.
Costa, F., Carvalho-Pereira, T., Begon, M., Riley, L., & Childs, J. (2017). Zoonotic and Vector-Borne Diseases in Urban Slums: Opportunities for Intervention. Trends Parasitol, 33(9), 660-662. https://doi.org/10.1016/j.pt.2017.05.010
Ernst, K. C., Phillips, B. S., & Duncan, B. D. (2013). Slums are not places for children to live: vulnerabilities, health outcomes, and possible interventions. Adv Pediatr, 60(1), 53-87. https://doi.org/10.1016/j.yapd.2013.04.005
Ezeh, A. P., Oyebode, O. P., Satterthwaite, D. P., Chen, Y.-F. P., Ndugwa, R. P., Sartori, J. B. A., Mberu, B. P., Melendez-Torres, G. J. P., Haregu, T. P., Watson, S. I. P., Caiaffa, W. P., Capon, A. P., & Lilford, R. J. P. (2016). The history, geography, and sociology of slums and the health problems of people who live in slums. Lancet, 389(10068), 547-558. https://doi.org/10.1016/S0140-6736(16)31650-6
Field, E. (2005). Property Rights and Investment in Urban Slums. Journal of the European Economic Association, 3(2/3), 279-290. https://doi.org/10.1162/1542476054472937
Galiani, S., Gonzalez-Rozada, M., & Schargrodsky, E. (2009). Water Expansions in Shantytowns: Health and Savings. Economica (London), 76(304), 607-622. https://doi.org/10.1111/j.1468-0335.2008.00719.x
Global Steering Group for Impact Investment. (2022). Informal Settlements: No Longer Invisible.
Gonzalez-Navarro, M., & Quintana-Domeque, C. (2016). PAVING STREETS FOR THE POOR: EXPERIMENTAL ANALYSIS OF INFRASTRUCTURE EFFECTS. The review of economics and statistics, 98(2), 254-267. https://doi.org/10.1162/REST_a_00553
Hutton, G., & Bartram, J. (2008). Global costs of attaining the Millennium Development Goal for water supply and sanitation. Bull World Health Organ, 86(1), 13-19. https://doi.org/10.2471/blt.07.046045
Kapse, V. S., Pofale, A. D., Mathur, M. J. I. j. o. h., & sciences, s. (2012). Paradigm of Relocation of Urban Poor Habitats (Slums): Case Study of Nagpur City. 6, 2916-2923.
Kuffer, M., Pfeffer, K., & Sliuzas, R. (2016). Slums from Space—15 Years of Slum Mapping Using Remote Sensing. Remote Sensing, 8, 455. https://doi.org/10.3390/rs8060455
Lilford, R. J., Oyebode, O., Satterthwaite, D., Melendez-Torres, G. J., Chen, Y. F., Mberu, B., Watson, S. I., Sartori, J., Ndugwa, R., Caiaffa, W., Haregu, T., Capon, A., Saith, R., & Ezeh, A. (2017). Improving the health and welfare of people who live in slums. Lancet, 389(10068), 559-570. https://doi.org/10.1016/s0140-6736(16)31848-7
Mahabir, R., Croitoru, A., Crooks, A. T., Agouris, P., & Stefanidis, A. (2018). A Critical Review of High and Very High-Resolution Remote Sensing Approaches for Detecting and Mapping Slums: Trends, Challenges and Emerging Opportunities. Urban Science, 2(1).
Mberu, B. U., Haregu, T. N., Kyobutungi, C., & Ezeh, A. C. (2016). Health and health-related indicators in slum, rural, and urban communities: a comparative analysis. Glob Health Action, 9, 33163. https://doi.org/10.3402/gha.v9.33163
Nolan, L. B., Bloom, D. E., & Subbaraman, R. (2018). Legal Status and Deprivation in Urban Slums over Two Decades. Econ Polit Wkly, 53(15), 47-55.
Titiunik, R., Martinez, S., Gertler, P., Galiano, S., & Cattaneo, M. (2007). Housing, Health, And Happiness. Research Working papers, 1, 1-34. https://doi.org/10.1596/1813-9450-4214
UN-HABITAT. (2003). Guide to Monitoring Target 11: Improving the lives of 100 million slum dwellers. https://unhabitat.org/sites/default/files/download-manager-files/Guide%20to%20Monitoring%20MDG%20Target%2011.pdf
UN-Habitat. (2022). Annual Report 2021. https://unhabitat.org/sites/default/files/2022/05/2021_annual_report.pdf
UN Habitat. (2020). Harsh Realities: Marginalized Women in Cities of the Developing World. https://unhabitat.org/sites/default/files/2020/06/harsh-realities-marginalized-women-in-cities-of-the-developing-world-en.pdf
United Nations. (2021). Report of the Advisory Committee on Administrative and Budgetary Questions on the draft work programme and budget of the United Nations Human Settlements Programme for the year 2022. https://unhabitat.org/sites/default/files/2021/10/english-202114.pdf
World Habitat. (2015). TECHO – Development of Habitat. https://world-habitat.org/world-habitat-awards/winners-and-finalists/techo-development-of-habitat/

Thanks for this! I did not realize 1 billion people currently live in slums.
Minor nitpick: The investigation is called shallow in the beginning, but in-depth in the end.
Thank you! Fixed now :)
Very well written post. Thank you for your work!
Thank you for this - it was a super interesting read and well written!