Read full report
Executive Summary
From the Plague of Justinian to the recent COVID-19 pandemic, infectious diseases have caused some of the largest death tolls in history. While many pathogens have existed for millennia, changes in human behavior have facilitated their spread. Human population growth, globalization, and environmental damage contribute to the development and spread of dangerous new human diseases known as emerging infectious diseases (EID), such as severe acute respiratory syndrome (SARS), AIDS, Ebola, dengue, or yellow fever. In fact, between 1940 and 2004, at least 335 EIDs have been identified. According to WHO data, a steady increase in EIDs has been observed during this period, indicating an upward trend that is expected to continue in the future.
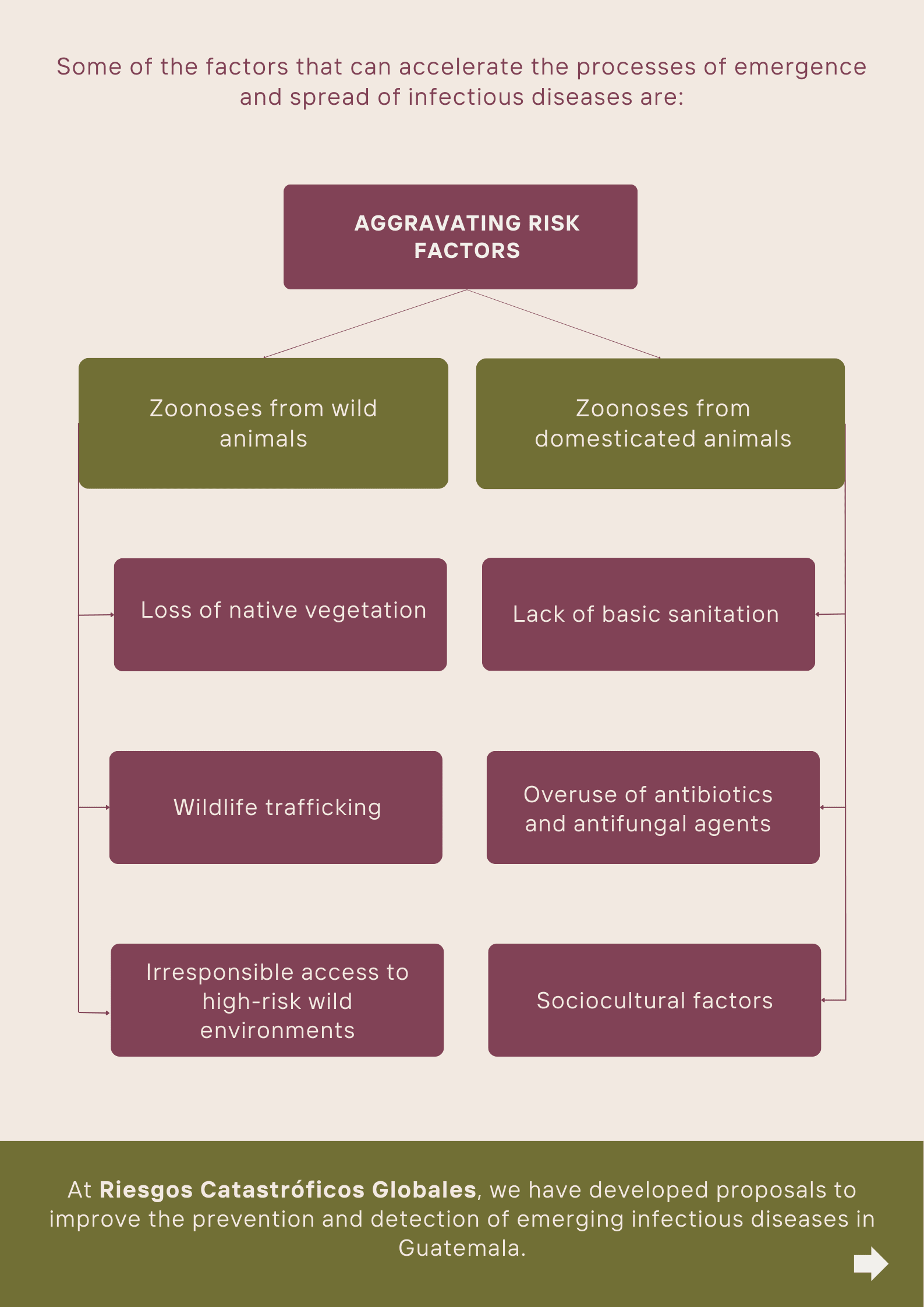
In recent years, most emerging human diseases have been transmitted by zoonotic pathogens – that is, those transmitted between animals and humans. Approximately 60.3% of EIDs in recent decades are estimated to have a zoonotic origin. That represents a significant challenge for public health.
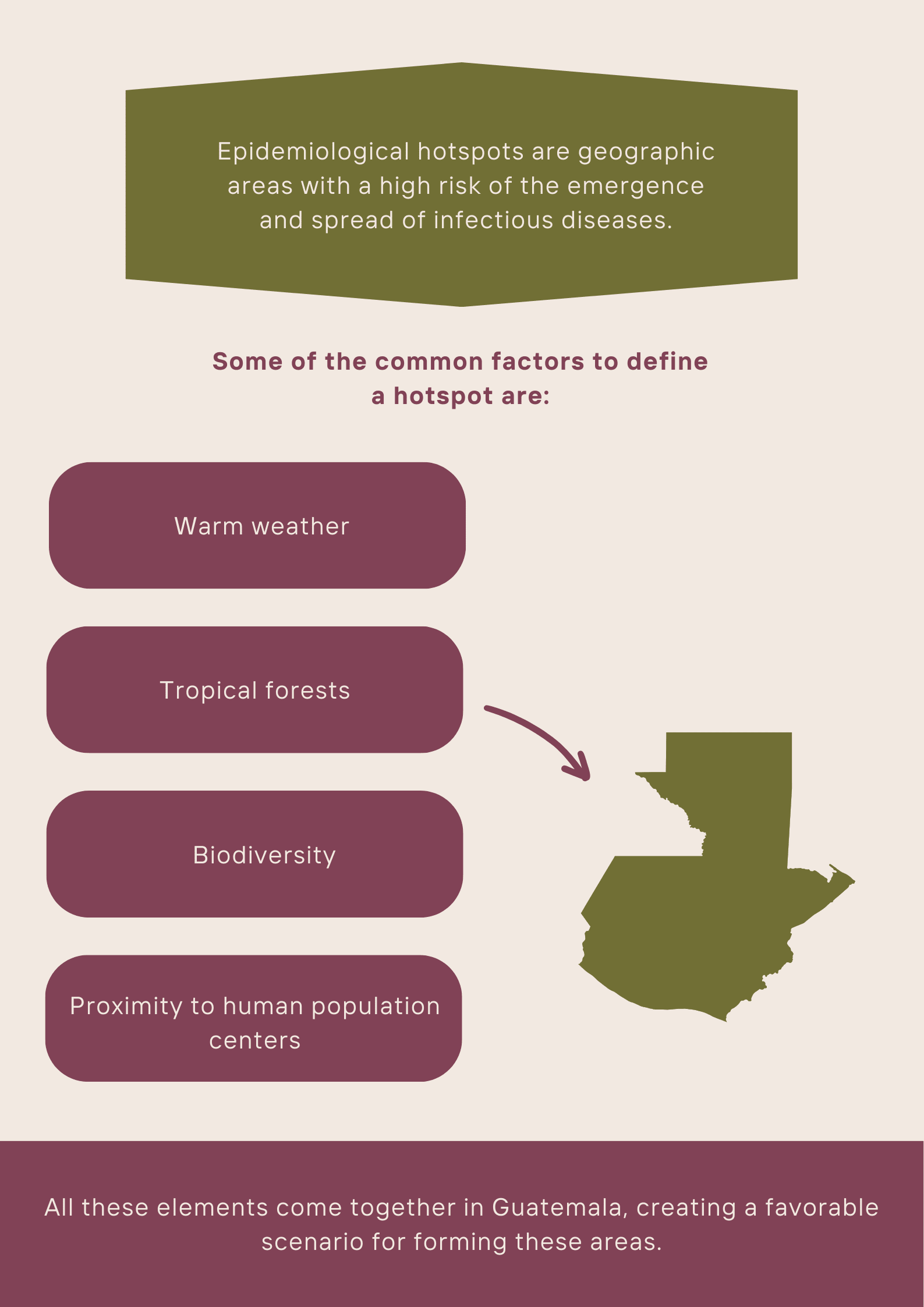
In this context, Guatemala emerges as a country of particular interest for our analysis since it has a combination of factors that favor the appearance of epidemiological hotspots. Among these factors are its warm climate, tropical forests, and wide variety of wild species, as well as the proximity of human population centers to natural habitats. That is in addition to rapid urbanization, unsustainable agricultural development, and high population density. Indeed, Central America is one of the fastest-growing urban regions in the world and Guatemala stands out with an annual urban population growth rate of 3.4%, making it one of the main drivers of this trend.
In turn, outbreaks of diseases such as dengue fever, Chagas disease, and avian influenza have been reported in Guatemala. This dynamic is partly fostered by livestock and poultry farming, both common in the Guatemalan rural population. 60% of the animal protein consumed by Guatemalans comes from local poultry farming, which is at risk of known diseases such as avian influenza or the West Nile virus. These outbreaks have been aggravated by poor health infrastructure in some areas. For example, poor access to sanitation services, especially in rural areas and among indigenous groups, contributes to the spread of infectious diseases. According to WHO and UNICEF data, approximately 44% of the Guatemalan rural population does not have access to basic sanitation, and almost half of the population in the country lacks access to improved sanitation.
Finally, in terms of investment in public health, Guatemala shows relatively low per capita spending compared to other countries in the region. In 2022, public expenditure on health stood at 82 euros per capita, while Costa Rica and Panama had per capita spending of 634 and 590 euros, respectively. Mexico spent 246 euros per capita, while other Central American countries ranged between 99 and 169 euros.
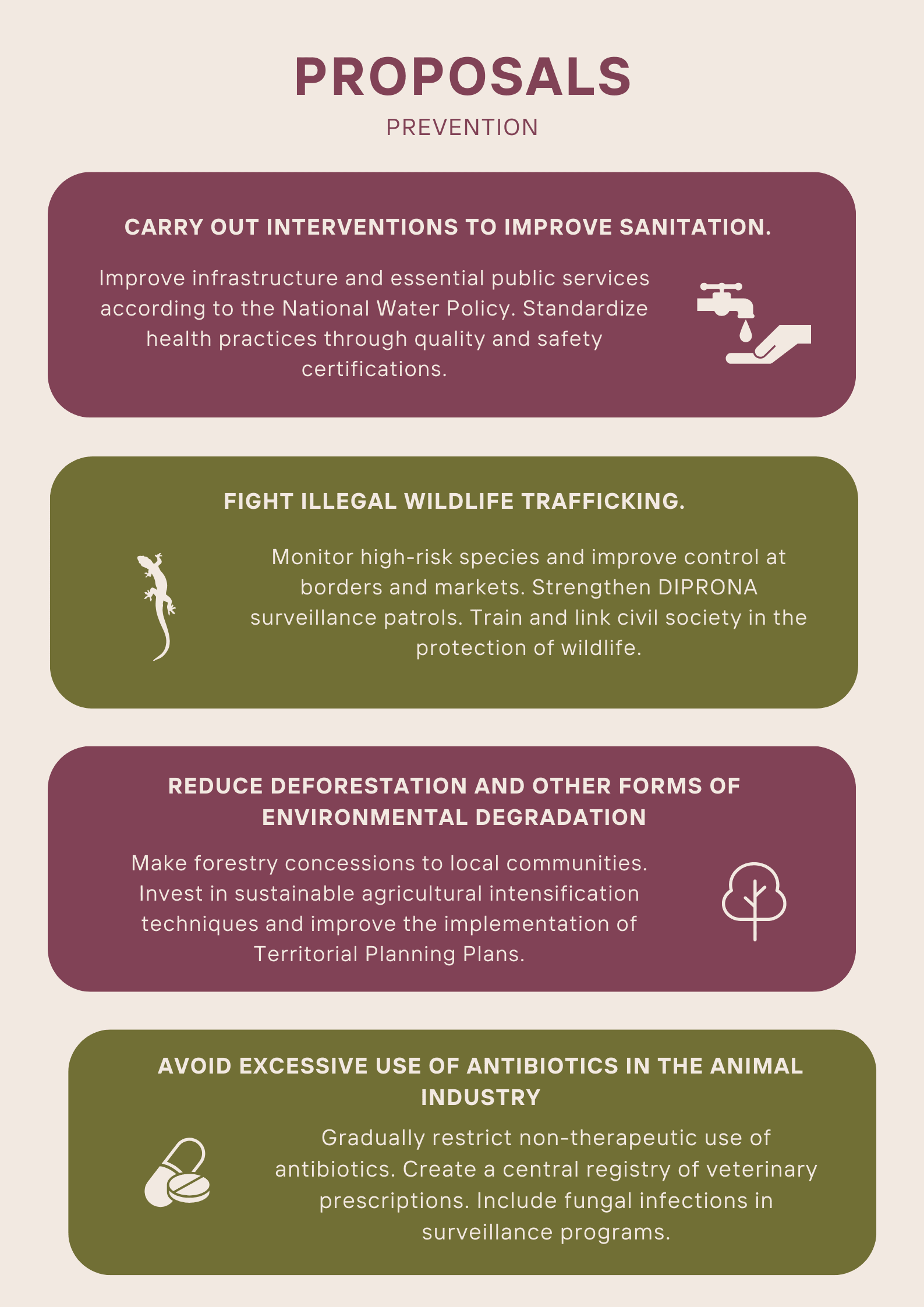
Considering these factors, we identify opportunities for improvement and offer recommendations to prevent and detect the development or spread of infectious diseases. As for prevention, we propose four objectives: first, improving sanitation through interventions in essential infrastructure, such as public water and waste services, as well as through sanitary measures when coming into contact with domesticated animals or wildlife; second, curbing illegal wildlife trade; third, halting deforestation and other forms of environmental degradation; and fourth, avoiding the abuse of antibiotics in the animal agriculture industry.
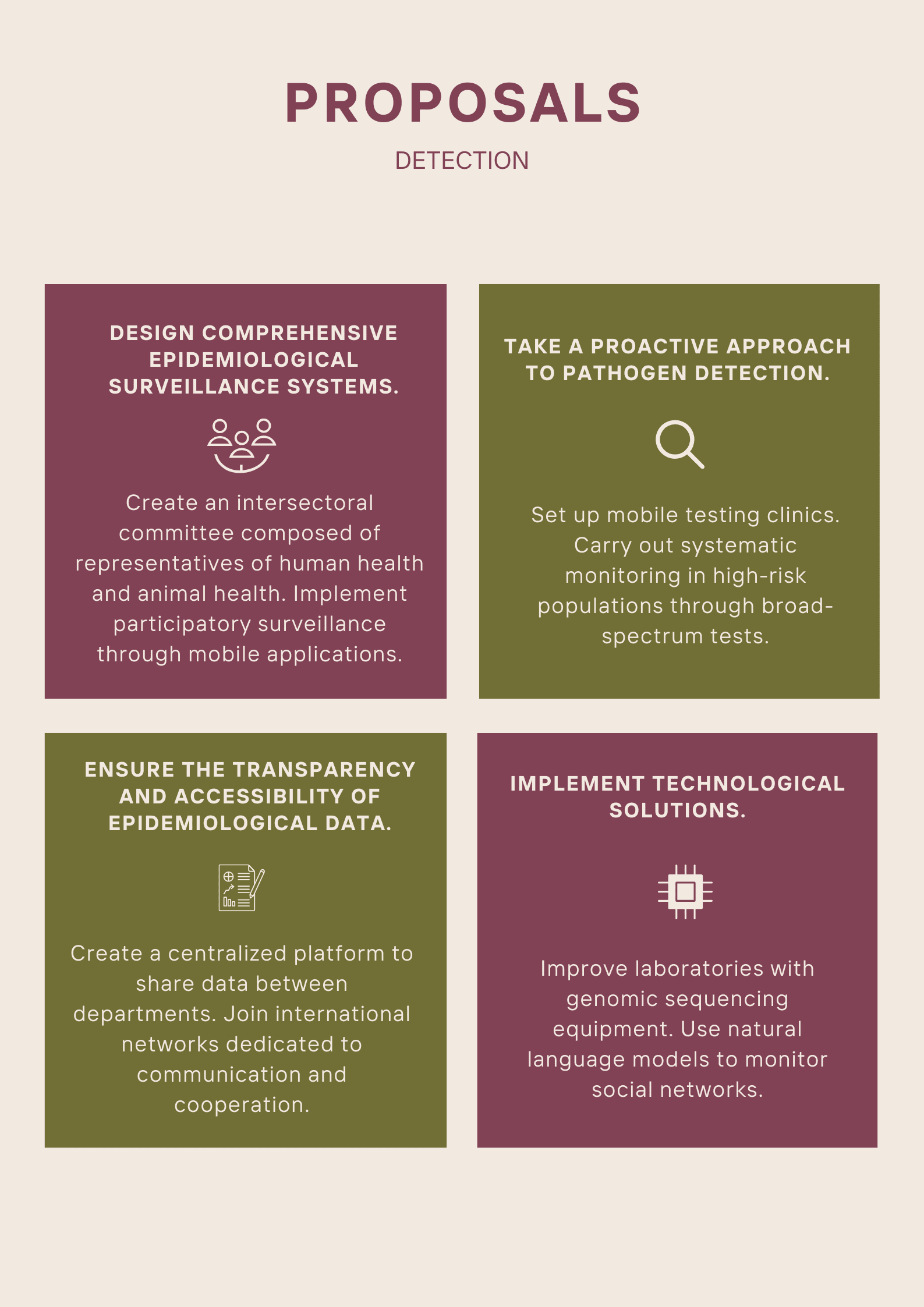
Regarding detection, we propose greater articulation of epidemiological surveillance systems — including improved coordination between the Ministry of Public Health and Social Assistance (MSPAS) and the Ministry of Agriculture, Livestock, and Food (MAGA) — as well as the increased participation of local communities. We also suggest implementing a proactive approach to detecting pathogens through systematic monitoring in high-risk populations and mobile testing clinics that carry out broad-spectrum tests in rural communities. Finally, we recommend improving the transparency and accessibility of the gathered data and implementing technological solutions such as genomic sequencing and natural language processing to track sources of infection on social media.
All these proposals are grounded in scientific literature and the interviews we conducted with experts in the field. Their implementation is feasible in the Guatemalan context and would benefit public health and other sectors without incurring excessive costs.
Infographic



Just wanted to give you a heads-up on a small tweak I made to the title of this post. The original title was in all caps so I went ahead and changed it to avoid slipping into ~clickbaity titles.
Thanks Dane :)