TLDR: NGOs and other health providers often fail to reach the remote communities where their impact could be highest. Our Health AIM tool helps NGO and government Health providers target their interventions more effectively, increasing the impact at less cost.
Introduction
I’m Emma Ochola, Co-Founder and regional manager of OneDay Health, an NGO which has launched 38 basic health centers in remote areas and treated over 150,000 patients. Our goal is that every rural citizen will have access to quality health care. On early stage analysis by my Co-Founder Nick, we estimate that OneDay Health may save lives cost-effectively. We at OneDay Health have developed Health AIM (Accessibility Identification Map), to help other health providers in Uganda and beyond reach underserved and neglected areas they would otherwise have ignored.
Even Highly Rated NGOs fail to reach remote, rural areas
In Uganda, 5 million people live in rural remote areas with poor access to health care. These rural people need to travel over 5 kilometers on foot or motorbike ‘boda boda’ to reach services such as primary healthcare, maternity and vaccination.
I was born in remote Kitgum District district, Northern Uganda. During my 34 year life, I have seen numerous NGOs and health providers fail to reach these remote rural poor as they implement countless healthcare projects and programs. These failures even involve some highly rated GiveWell charities, including AMF supported mosquito net distribution, Malaria consortium supported ACT distribution and deworming programs. Their programs reach rural areas, but rarely the most remote places.
Sadly, those missed by NGOs are those are likely to already have the worst health outcomes and would have benefited the most from these programs. When NGOs neglect these remote rural areas, they fail to maximise their impact
Why do Health Providers fail to reach those most in need?
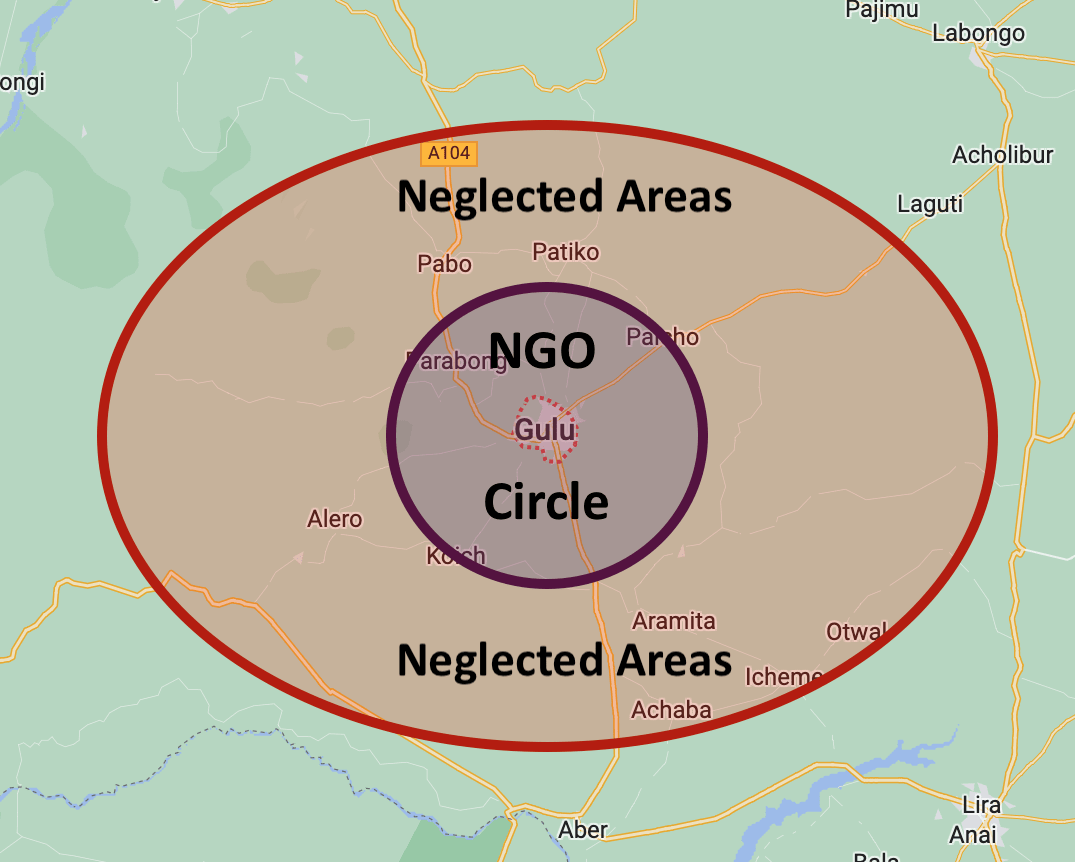
The one hour “NGO circle”
At a very loose guess perhaps 80% of NGO effort reaches 20% of the population here in Northern Uganda. Most NGOs have their bases in large towns or cities. Where I live in Gulu, NGO offices are abundant and they spend most of their money and time within about an hours drive from town. As you start to drive out of town, NGO signs abound, then the deeper in the village you reach they fade away. NGOs love to be able to drive to their worksite within an hour or so, do their training or other work, then drive back to town to their comfortable homes and offices. Remote areas are sometimes reached but often are neglected. I wonder if this phenomenon exists in other places too.
Out of sight, out of mind
“See no evil, hear no evil, speak no evil” The majority of NGO and government health providers are somewhat aware that they are not reaching large populations in more remote areas, but it is easy to ignore places you never reach and never see with your own eyes. Our Health AIM tool can help remove this excuse.
Lack of Incentives to reach the areas most in need
Most NGOs have key metrics of numbers and stories. Who exactly you reach may not be so important, How Many is the big metric = the figure reported to donors and the public. Yes these NGOs reach poor people, but not those most in need. Stories can help show the kind of people being helped, but they often fail to show the difference between the poor and the very poor. NGOs therefore aren’t incentivised to serve the 5% or 10% of people who would may benefit from the most from their intervention.
Stories illustrating failure to reach the last mile
Example 1 – Mosquito net distribution
Seven years ago, when I was in my final year at nursing school I interned in a remote area in Pabbo subcounty. I witnessed a strange distribution of mosquito nets. The nets were distributed from the subcounty headquarters and the majority of the beneficiaries were people from the urban centres. They failed to reach the remote rural population where they could have had the most impact. Many of the nets distributed were even sold echeaply at the trading centres inchange for food items.
Story 2 – Maternity project
In 2019, we launched a new OneDay health Centre in Te Olam, a remote area far from government health Centres. At that time a USAID voucher project targeted pregnant mothers, funding their antenatal care and delivery. The project was well designed for the rural poor but all of the Te Olam area was missed, because the project had no nearby large health center to distribute vouchers. There were some outreach efforts from the nearest health facility, but for the reasons outlined above, Te Olam was ignored and mothers there didn't get the help they needed
Considering these issues prompted our OneDay Health team to create “Health AIM”, to put these neglected areas on the map and compel healthcare providers to consider and not ignore remote areas.
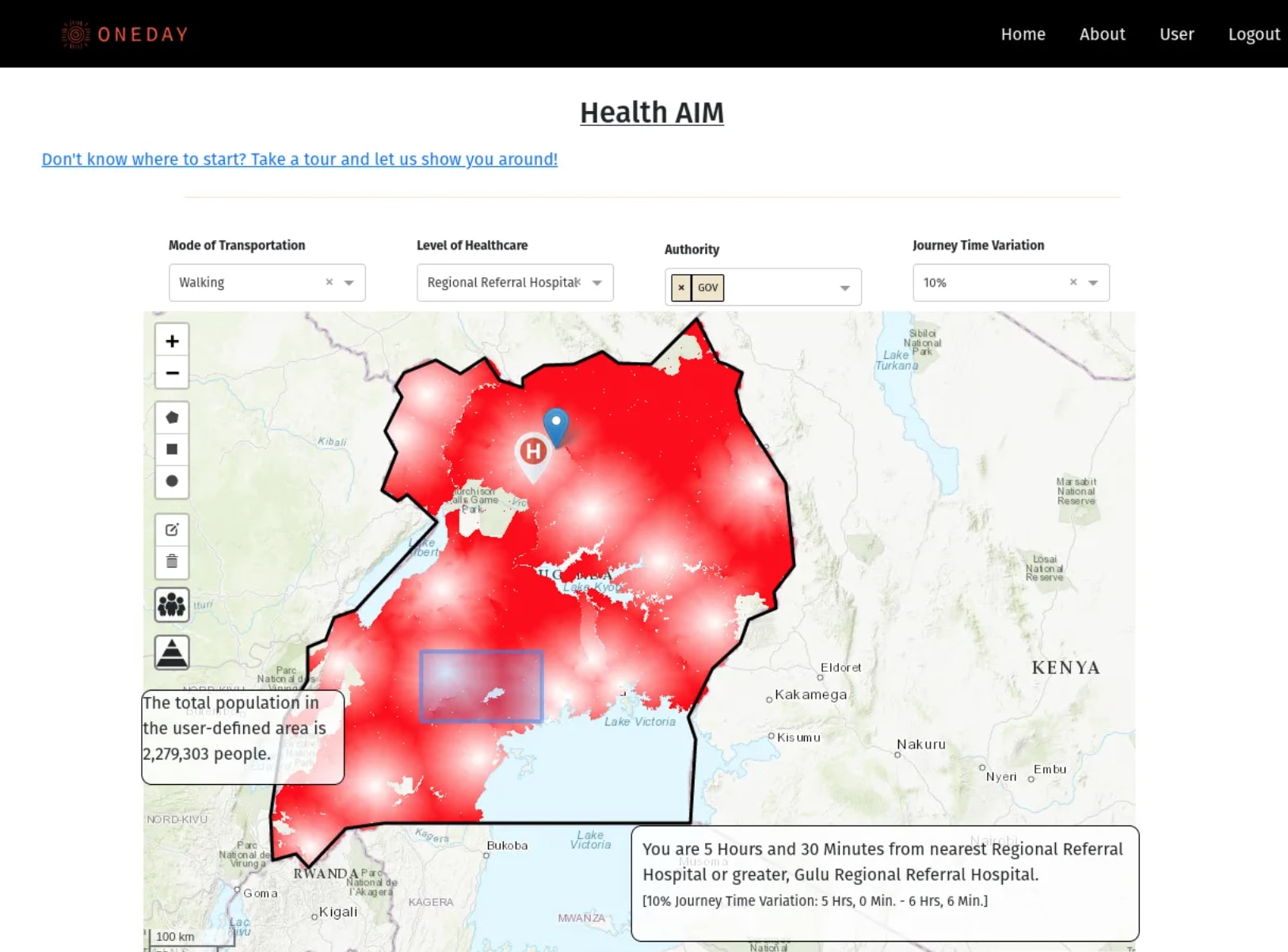
Health AIM – Helping organisations reach underserved areas
Health AIM is an interactive mapping tool which identifies remote rural communities with poor access to healthcare, and illustrates specific health needs of those communities. Government, private and international health partners can use HealthAIM to target underserved remote communities they may previously have neglected. Health Aim empowers health providers to improve their cost effectiveness through prioritising healthcare to neglected communities, and allocating resources where they are most needed.
Give Health AIM a try and see what you think
https://health-aim.onedayhealth.cloud/
Health AIM Data Inputs
Health AIM integrates 4 publicly available data sources (more pending) to produce a Healthcare accessibility heatmap, with darker red indicating poorer access to healthcare.
1. All Government (and most private) health facilities are located, classified based on the level of care they offer
- Health center II = primary healthcare
- Health center III = maternity care
- Health center IV/Hospital = basic operations such as Cesarian section possib
2. Road networks are mapped, considering 3 levels of road quality. Primary roads were large, paved highways which connect international borders, secondary roads fed into or were connected to primary roads and connected major towns around the country, and tertiary roads were connected to secondary roads and connected small towns or market centers.
3. Population dataset was taken from Worldpop, which combines both census data and satellite images to estimate population down to 100x100 meter units.
4. Geographical barriers such as hills and water sources are also taken into consideration.
Features of Health AIM
- Countrywide heat maps identify communities with poor access to different levels of healthcare services, including primary care, maternity care and hospital level care
-One click anywhere on the map estimates the travel time needed to reach the nearest health facility through different transport modes of walking, biking and driving.
- Polygon selection tool estimates the population of user-defined areas, with multiple areas able to be selected and added at the same time
-Demographic pyramid tool estimates the number of people in different demographics in a selected area, for example children under 5 years old or women of child bearing age
- Interactive health center location map shows almost every health facility location in Uganda (not yet activated sorry!)
Improves cost-effectiveness
Health AIM could improve cost effectiveness of health provision organisations through a number of mechanisms, here are just a few.
- Reduced planning costs. Health AIM can help you identify potential large or small areas where health provision projects could have the most impact. This could save money on field visits
- Accurate resource allocation. More granular population based allocation of human resources such as Community Health Workers, or medical resources such as bednets or malaria commodities could help reduce wastage and better meet demands
- Improved monitoring. Health AIM could be used to help verify which areas have been reached or missed in a project.
- Remote areas seen and reached. Once remote underserved areas are clearly seen on a map, they are much harder to ignore. If Health AIM could facilitate a small (5-10%) reallocation of resources in a large project from less neglected areas to the most neglected places, cost effectiveness of projects could greatly increase
Potential Use Cases
- Accurately identify communities most in need of new or upgraded health facilities
-Ensure that mosquito net distributions reach the most remote areas, so no family misses out
-Help community health workers reach women with poor access to antenatal care
-Ensure equitable government distribution of medications, tests and health workers
Implementation Plan
We plan to demonstrate the power of Health AIM to NGO and government providers, highlighting neglected communities and work with partners to integrate Health AIM into their healthcare provision. This will empower healthcare providers to reach neglected populations that were previously ignored, improve universal health coverage and reduce healthcare inequalities
How you can help
- Try Health AIM and give us your honest opinion on how how usable and useful you think it could be
- We would love to talk with top charities such as AMF and Deworrm the world, to understand what current mapping tools they are currently using to help them target their work, and see if Health Aim could help them do it better.
- Health AIM was mostly developed on volunteer time on an absolute shoestring – moderate funding will help us add more features such as disease prevalence, vaccination coverage and potentially new geographies. If you have a specific use-case that could help your org reach remote rural areas and improve your cost-effectiveness, we would love to discuss building that for you
- We would love to have conversation with health map-tech people to explore the best way to promote and distribute Health AIM – thanks to Arnon Houri-Yafin of Zzapp for giving us great advice already.

This is super exciting, interesting work. I'd love to know what kind of stuff already exists in this space because it seems such a great way forward I'm surprised that we aren't more aware of it.
Do you think this mapping tool was only possible because of the in-depth local knowledge of Uganda the two of you bring? Or is this something that you could scale to other countries? Or could be done by desk-based researchers elsewhere?
I have also done some NGO/charitable/public sector mapping in Uganda and just remember it being an absolute nightmare driving around trying to work out which places were still open, had ever existed, or were open to our user base. Huge props to you guys for doing this work and I'm interested to follow its progress when you start talking to other orgs :)
Thanks, Joseph for the great question.
Health AIM can definitely be used by desk-based researchers, even if you have never been to Uganda our tool can help you understand the healthcare situation here.
The idea for the prototype came through our in-depth knowledge of the health service demand in Northern Uganda, and our mission to reach every healthcare "black hole" with quality healthcare. Now that we have this tool, scaling Health AIM to other countries is very doable because the underlying population and road network data would come from the same source - and we hope it will happen.